Introduction
‘It takes a child one year to acquire independent movement and ten years to acquire independent mobility. An old person can lose both in a day’
Professor Bernard Isaacs
(1924–1995)
This poignant quote from Professor Bernard Isaacs encapsulates the devastating impact a single fall can have on an older adult’s life. Falls, while common across all age groups, pose a particularly significant threat to individuals aged 65 years and older. Despite ongoing research and clinical efforts, approximately 30% of older adults experience a fall annually, often leading to severe consequences that extend beyond physical injury. These incidents contribute to a cascade of negative outcomes, including increased morbidity, disability, hospitalization, institutionalization, and even mortality. The global burden of falls is staggering, with the Global Burden of Disease study reporting nearly 17 million years of life lost in 2017 alone. Economically, falls-related expenditures account for approximately 1% of healthcare costs in high-income countries, highlighting the substantial societal and financial implications.
The prevalence of falls and related injuries is projected to rise further due to the global aging population and the increasing incidence of multimorbidity, polypharmacy, and frailty among older adults. Geographical variations in falls prevalence exist, potentially influenced by cultural and lifestyle factors. For instance, rates among ethnic Chinese populations in Southeast Asia range from 15% to 34%, while Latin American and Caribbean regions report rates between 22% and 34%. Furthermore, falls are more frequent in specific settings such as care homes and hospitals, suggesting that risk factors and preventative strategies may need to be tailored to these environments.
The Imperative for Updated Falls Prevention Guidelines
Recognizing the escalating global challenge of falls in older adults, a consensus emerged among 14 international experts in 2019 to establish the World Falls Guidelines (WFG) Task Force. This initiative stemmed from the understanding that existing national and specialist guidelines were becoming outdated and inconsistent in light of new research and evolving clinical service demands. A comprehensive systematic review confirmed these gaps and inconsistencies, underscoring the necessity for a new set of clinical practice guidelines with a global perspective. These updated guidelines aim to address the shortcomings of previous recommendations and incorporate the latest advancements in falls prevention and management.
 Bernhard Isaacs Quote
Bernhard Isaacs Quote
In 2019, the National Institute for Health and Care Excellence (NICE) in England also recognized the need to update its 2013 guidelines. Their systematic assessment concluded that new evidence, accumulated up to February 2019, significantly impacted case-finding, falls risk assessments, and preventative interventions. Since then, a substantial body of research has emerged, remaining largely unevaluated within existing guideline frameworks. Observational studies have refined our understanding of risk stratification in community-dwelling and clinical populations. Mechanistic and epidemiological research has deepened our knowledge of falls in older adults with cognitive impairment. Moreover, the advent of e-health technologies, including wearables, virtual reality applications, and environmental monitoring devices, presents novel opportunities for falls prevention that were not considered in prior guidelines.
Falls are disproportionately prevalent in clinical care settings such as hospitals, rehabilitation units, assisted living facilities, and care homes. Current clinical practice guidelines often lack comprehensive coverage of the specific risk factors and management strategies relevant to these settings. However, recent evidence specific to these environments provides a foundation for developing targeted recommendations. Furthermore, previous guidelines have inconsistently incorporated the perspectives of older adults, caregivers, and other stakeholders. Emerging evidence emphasizes the importance of these viewpoints in shaping the suitability and feasibility of guideline recommendations, ensuring that interventions are person-centered and effectively address the needs and preferences of older adults.
Purpose and Scope of the 2019 World Falls Guidelines
The overarching goal of these 2019 World Falls Guidelines (WFG) is to contribute to the global effort to improve the health and well-being of older adults, aligning with the United Nations Decade of Healthy Ageing (2021–2030). Healthy aging is defined as maintaining the functional ability to engage in activities and roles that individuals value. Reducing falls and fall-related injuries, particularly fractures and head injuries, is crucial for preserving functional mobility and alleviating concerns about falling, which can significantly limit activity and quality of life. Therefore, the primary objective of the WFG is to provide evidence-based guidelines for healthcare professionals and other stakeholders working with older adults. These guidelines offer comprehensive strategies for identifying and assessing falls risk, and recommend effective interventions, both individually and in combination, within a person-centered care framework.
These guidelines are groundbreaking in their systematic consideration of several key aspects:
- Person-centered approach: Integrating the lived experiences and perspectives of older adults, caregivers, and other relevant stakeholders to ensure interventions are tailored to individual needs and preferences.
- Addressing gaps in previous guidelines: Rectifying inconsistencies and omissions identified in earlier national and international guidelines, ensuring comprehensive coverage of current best practices.
- Integration of e-health advancements: Incorporating recent developments in e-health technologies to enhance falls prevention strategies and leverage digital tools for assessment and intervention.
- Implementation in diverse settings: Addressing the challenges of implementing falls prevention programs in various settings, including resource-constrained environments and low- and middle-income countries (LMICs).
The 2019 WFG adopts the World Health Organization’s definition of a fall: “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level. Falls, trips and slips can occur on one level or from a height.” This definition encompasses syncopal events, acknowledging the diverse nature of falls. While the guidelines primarily target individuals aged 65 years and older, they recognize that in certain contexts, age 60 may be a more appropriate threshold depending on health expectancies and local considerations. The research evidence underpinning these guidelines includes studies with varying age ranges, reflecting the complexity of defining “older age” in a strictly chronological manner.
The guidelines focus on individual-level actions and are intended for older adults living in the community, care homes, and hospitals. They also address specific assessment and prevention strategies for older adults with common medical conditions associated with increased falls risk, such as Parkinson’s disease (PD), post-stroke conditions, post-hip fracture recovery, and significant cognitive impairment. Distinct recommendations are provided for these populations where evidence supports tailored approaches.
Recognizing the unique challenges of implementing falls prevention guidelines in LMICs, where access to human and technical resources may be limited, the 2019 WFG explicitly addresses these considerations. The guidelines acknowledge that risk factors and effective interventions may differ in LMICs compared to high-income countries, and therefore incorporate these factors into recommendations and implementation advice. While the management of fall-related injuries is outside the scope of these guidelines, they emphasize the critical link between falls and fragility fractures. The WFG advocates for seamless integration with clinicians and services specializing in bone health, osteoporosis, and fracture risk management, referencing existing multilingual guidelines in these areas.
Utilizing the 2019 Falls Prevention Guidelines in Practice
The 2019 World Falls Guidelines are designed for a broad range of healthcare professionals, including physicians, nurses, physiotherapists, occupational therapists, pharmacists, and allied health professionals. Effective implementation necessitates collaborative efforts across various healthcare and social care sectors, from non-specialist to specialist levels. Service design should facilitate care pathways that connect primary and community services with specialist resources as needed. While adaptation to local contexts, healthcare systems, and resource availability is essential, the core recommendations are intended to be globally applicable to older adult populations. Population-level public health initiatives and community-level actions, such as environmental design and age-friendly communities, which indirectly impact falls rates, are beyond the immediate scope of these guidelines but are recognized as important complementary strategies.
The guidelines promote a flexible, person-centered approach to falls prevention, characterized by four key principles:
- Predictive: Utilizing available information to assess an individual’s risk of falls and fall-related injuries, enabling proactive risk stratification.
- Preventative: Focusing on interventions and strategies designed to prevent falls and related injuries while simultaneously optimizing functional ability and overall well-being.
- Personalized: Tailoring interventions based on identified fall risk factors and other relevant clinical information, such as cognitive status, to create individualized prevention plans.
- Participatory: Emphasizing collaborative goal setting and plan development, involving the older adult and their chosen support network to consider priorities, values, and available resources, including caregiver support.
Development Process of the 2019 World Falls Guidelines
The rigorous development process of the 2019 World Falls Guidelines is detailed in Appendix 1 of the full publication in Age and Ageing. The World Falls Guidelines Task Force comprised 96 experts from 39 countries across five continents, representing 36 scientific and academic societies. A Steering Committee provided strategic direction and oversight throughout the project. Crucially, the guidelines development incorporated feedback from older adults from the outset, ensuring that their perspectives shaped the recommendations to better meet the needs of older adults in community and long-term care settings.
A systematic review conducted in 2020 analyzed existing falls prevention and management guidelines, identifying critical gaps and areas of controversy. These findings informed the creation of 11 topic-specific working groups (WGs) to address these knowledge gaps. Each WG developed preliminary graded recommendations based on systematic reviews, as detailed in their individual WG reports in Appendix 2. A separate WG focused on integrating the perspectives of older adults as a cross-cutting theme. Additionally, ten ad hoc expert groups conducted rapid reviews of clinical areas not covered by the primary WGs. An international Experts Group provided external review and feedback on the preliminary and revised recommendations through a four-stage modified Delphi process. This iterative process culminated in a final vote on the recommendations by Steering Committee members and WG leaders, informed by structured feedback from a panel of older adults.
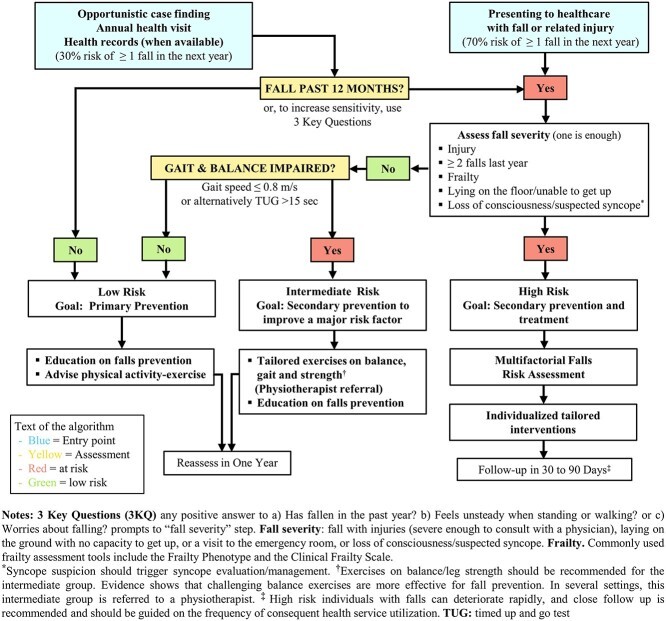
Furthermore, an ad hoc WG of eight clinician experts developed a practical falls assessment and management algorithm, integrating risk stratification, assessment, and interventions based on the evidence synthesized by the WGs. Appendix 4b lists the full membership of all committees and WGs, acknowledging the extensive collaborative effort involved in creating these guidelines.
The grading of recommendations follows a modified version of the widely used Grading of Recommendations, Assessment, and Evaluation (GRADE) criteria (Table 1). This system assesses both the strength of the recommendation (1 for strong, 2 for weak-conditional) and the quality of the supporting evidence (A for high, B for intermediate, C for low). In situations where evidence was lacking but a recommendation was deemed necessary, the modified GRADE system allowed for a grade of ‘E’ (expert consensus advice recommendation) (Tables 2 and 3).
Table 1. Modified GRADE System for Recommendation Strength and Evidence Quality
| Strength of Recommendation | 1 | Strong: Benefits clearly outweigh undesirable effects, indicating a high level of confidence in the recommendation. |
|---|---|---|
| 2 | Weak or conditional: Evidence quality is lower, or desirable and undesirable effects are more closely balanced, suggesting less certainty in the recommendation. | |
| Quality of evidence | A | High: Further research is unlikely to significantly alter the confidence in the estimated effect, indicating robust evidence. |
| B | Intermediate: Further research is likely to have a notable impact on confidence in the estimated effect and may potentially change the estimate, suggesting moderate evidence. | |
| C | Low: Further research is very likely to substantially impact confidence in the estimated effect and is likely to change the estimate, indicating limited evidence. | |
| No evidence Available | E | Experts: Recommendation formulated based on expert consensus when evidence was lacking or of insufficient quality. |
Table 2. Taxonomy of Terms Used in the 2019 World Falls Guidelines
| Term | Definition |
|---|---|
| Fall | An unexpected event in which an individual unintentionally comes to rest on the ground, floor, or another lower level. |
| Recurrent falls | Experiencing two or more falls within the preceding 12 months, indicating a pattern of falling. |
| Unexplained fall | A fall where no apparent cause is identified after a comprehensive multifactorial falls risk assessment, and it cannot be attributed to environmental hazards or gait/balance abnormalities. |
| Severe fall | A fall resulting in injuries severe enough to necessitate medical consultation, causing prolonged inability to get up from the floor (at least one hour), requiring emergency room visit, or associated with loss of consciousness. |
| Fall related injury | Any injury sustained as a consequence of a fall, requiring medical attention, including hospitalization for conditions like fractures, dislocations, head injuries, sprains, strains, bruises, lacerations, or other serious injuries. |
| Fall risk stratification | A process using single or multiple assessments to categorize an individual’s risk of falling, guiding subsequent assessment and intervention strategies. |
| Multifactorial falls risk assessment | A comprehensive evaluation across multiple domains to determine an individual’s overall fall risk and identify specific modifiable and non-modifiable risk factors that inform intervention choices. |
| Caregiver | An individual who provides assistance with daily needs to another person. Caregivers can be formal (paid professionals with training, e.g., home health aides) or informal (unpaid family members or friends). |
| Exercise | A planned, structured, and repetitive subset of physical activity aimed at improving or maintaining physical fitness, encompassing health-related and skill-related attributes. |
| Fall risk increasing drugs (FRIDs) | Medications known to elevate the risk of falls due to their potential side effects on balance, cognition, or cardiovascular function. |
| Fall risk stratification algorithm | A systematic decision-making process and intervention pathway for case findings related to falls risk, guiding appropriate responses based on risk level. |
| Low- and Middle- income countries (LMIC) | Countries classified by the World Bank as low- and middle-income economies, facing unique resource and infrastructure challenges in healthcare delivery. |
| Multicomponent exercise | Exercise programs integrating strength, aerobic, balance, gait, and flexibility training to address multiple physical domains simultaneously. |
| Multidomain interventions | Interventions combining two or more components across different domains (e.g., exercise and environmental modifications), tailored based on multifactorial falls risk assessment to prevent or minimize falls and related injuries. |
| Multicomponent interventions | Fixed combinations of two or more intervention components, not individually tailored following a multifactorial assessment, and may include medication review, home modifications, and generic exercise advice. |
| Physical activity | Any bodily movement produced by skeletal muscles resulting in energy expenditure, encompassing occupational, sports, conditioning, household, and other daily activities. |
| Telehealth | Utilizing telephone or video calls to communicate with individuals at home, enabling remote healthcare delivery and monitoring. |
| Smart home systems | Technology-driven systems employing sensors and Artificial Intelligence (AI) to reduce environmental hazards and predict potential falls in home settings. |
Table 3. Acronyms Used in the 2019 World Falls Guidelines Text
| Acronym | Full Term |
|---|---|
| 3IQ | Three Incontinence Questionnaire |
| 3KQ | Three Key Questions |
| ADL | Activities of Daily Living |
| BMI | Body mass index |
| CFS | Clinical Frailty Scale |
| CGA | Comprehensive geriatric assessment |
| CST | Chair Stand Test |
| DT | Dual tasking |
| FES-I | Falls Efficacy Scale International |
| FOG | Freezing of gait |
| FP | Frailty phenotype |
| FRIDs | Fall risk increasing drugs |
| GDS | Geriatric Depression Scale |
| GRADE | Grading of Recommendations, Assessment, and Evaluation |
| IADL | Instrumental Activities of Daily Living |
| ICFSR | International Conference on Frailty and Sarcopenia |
| LMIC | Low- and middle-income countries |
| MCI | Mild Cognitive Impairment |
| MDS-UPDRS | Movement Disorders Society Unified Parkinson’s Disease Rating Scale |
| MNA | Mini Nutritional Assessment |
| MoCA | Montreal Cognitive Assessment |
| NEADL | Nottingham Extended Activities of Daily Living |
| NICE | National Institute for Health and Care Excellence |
| NSAIDs | Non-steroidal anti-inflammatory drugs |
| PD | Parkinson’s Disease |
| RCT | Randomized controlled trial |
| Short FES-I | Short Falls Efficacy Scale International |
| SNRIs | Serotonin norepinephrine reuptake inhibitors |
| SPPB | Short Physical Performance Battery |
| TMT | Trail Making Test |
| TMT-B | Trail Making Test Part B |
| TUG | Timed Up and Go |
| WFG | World Falls Guidelines |
| WGs | Working groups |
Framework of the 2019 Falls Prevention Guidelines
The 2019 World Falls Guidelines are structured around a comprehensive framework encompassing four key stages:
- Fall Risk Stratification: Implementing a standardized approach to estimate an individual’s level of falls risk, guiding the intensity and detail of subsequent assessment and intervention.
- Assessment: A thorough process of identifying and quantifying falls risk factors across multiple domains, utilizing recommended assessment tools to pinpoint modifiable areas for intervention. Integrated with other components of a comprehensive geriatric assessment (CGA), this ensures a person-centered approach.
- Management and Interventions: Describing a range of falls prevention approaches, including recommended treatments and actions, suitable as single interventions or in combination, to effectively reduce falls risk.
- Assessment and Treatment Algorithm: A practical algorithm linking the stages of risk stratification, assessment, and management, emphasizing a person-centered approach to designing individualized intervention plans.
Key Messages of the 2019 World Falls Guidelines
The 2019 World Falls Guidelines emphasize several critical messages for effective falls prevention and management:
- Global Aging and Falls: The world’s aging population is leading to an increasing prevalence of falls and related injuries, making falls prevention a critical global public health challenge.
- Preventability of Falls: Many falls are preventable through evidence-based interventions and proactive management strategies, highlighting the importance of early identification and intervention.
- Multidisciplinary Management: Effective falls and injury prevention requires a multidisciplinary approach, involving collaboration among healthcare professionals, older adults, caregivers, and other stakeholders.
- Engaging Older Adults: Engaging older adults in falls prevention is essential. Understanding their beliefs, attitudes, and priorities regarding falls and their management is crucial for successful intervention implementation and adherence.
- Broader Benefits of Risk Factor Management: Addressing falls risk factors, such as gait and balance problems, yields broader health benefits beyond falls prevention, including improvements in intrinsic capacities (physical and mental health), functional abilities, and overall quality of life.
- Feasibility of Risk Assessment: Trained clinicians can effectively assess future falls risk using simple, readily available resources, making falls risk screening and stratification accessible in various settings.
- Effectiveness of Multidomain Interventions: Multidomain interventions, tailored to individual risk factors, are effective in reducing falls rates among high-risk community-dwelling older adults, underscoring the importance of personalized care plans.
- High Risk in Care Settings: In care homes and hospital settings, all older adults should be considered at high risk of falls, necessitating comprehensive assessment and multidomain interventions as standard practice.
- Targeted Vitamin D Supplementation: Vitamin D supplementation for falls prevention should be reserved for individuals at risk of vitamin D deficiency, rather than universal supplementation, to optimize resource utilization and effectiveness.
- Condition-Specific Modifications: Assessment and intervention approaches may require modifications for older adults with specific medical conditions associated with increased falls likelihood, highlighting the need for tailored strategies.
- Adaptation for Resource-Limited Settings: The application of these guidelines may need to be adapted to meet the specific needs and resource constraints of older adults in low-resource settings and LMICs, ensuring global applicability and equity.
Falls Risk Stratification and Algorithm: Identifying Individuals at Risk
Building upon the seminal guidelines from the AGS/BGS/AAOS panel on falls prevention and management (2001, updated 2011), the 2019 World Falls Guidelines introduce a refined falls prevention and management approach and algorithm specifically for community-dwelling older adults. This algorithm stratifies falls risk into three categories, guiding appropriate interventions based on risk level:
- Low Risk: Older adults at low risk of falls should receive education on falls prevention and be encouraged to engage in exercise for general health and falls prevention benefits if interested.
- Intermediate Risk: In addition to education, older adults at intermediate risk should be offered targeted exercise programs or physiotherapy referrals to improve balance and muscle strength, thereby reducing their falls risk.
- High Risk: Older adults at high risk of falls require a comprehensive multifactorial falls risk assessment to inform individualized, tailored interventions addressing their specific risk factors.
Risk categorization should be conducted during routine opportunistic case-finding or when older adults present with a fall or fall-related injury, ensuring proactive identification of individuals who could benefit from preventive measures.
Opportunistic Case-Finding: Proactive Identification of Falls Risk
Strong Recommendation. Clinicians should proactively inquire about falls during routine interactions with older adults, as falls are often underreported and may not be spontaneously disclosed. GRADE: 1A.
Expert Recommendation. Older adults engaging with healthcare services for any reason should be asked at least annually about: (i) experiencing one or more falls in the past 12 months, and (ii) the frequency, characteristics, context, severity, and consequences of any falls. GRADE: E.
Expert Recommendation. When resources and time permit, clinicians should additionally inquire about (iii) experiences of dizziness, loss of consciousness, or gait/balance disturbances, and (iv) concerns about falling leading to activity limitations. GRADE: E.
Strong Recommendation. Older adults who report any of the above should undergo an objective gait and balance assessment to differentiate between low, intermediate, and high falls risk as part of initial risk stratification. GRADE: 1A.
Recommendation Details and Justification
Opportunistic case-finding is crucial because older adults may not proactively report falls due to various reasons, including fear of losing independence or minimizing the significance of falls. Routine inquiry normalizes the conversation around falls and encourages disclosure, enabling timely intervention. Annual screening aligns with the natural progression of falls risk factors and provides a practical timeframe for recollection. Including questions about dizziness, balance issues, and fear of falling enhances the sensitivity of case-finding, capturing a broader spectrum of individuals at risk. Objective gait and balance assessments are essential for accurate risk stratification and guiding appropriate intervention pathways.
Older Adults Presenting with Falls or Related Injuries: Responding to Fall Events
Expert Recommendation. Older adults presenting with a fall or related injury should be questioned about the details of the event, its consequences, history of previous falls, transient loss of consciousness or dizziness, pre-existing mobility impairments, and concerns about falling limiting activities. GRADE: E.
Expert Recommendation. An adult who sustains an injury requiring medical treatment (including surgery), reports recurrent falls (≥2) in the past 12 months, was unable to rise independently for at least one hour after a fall, is identified as frail, or is suspected of experiencing transient loss of consciousness should be considered at high risk of future falls. GRADE: E.
Recommendation Details and Justification
When an older adult presents with a fall, a thorough assessment of the event and individual risk factors is paramount. Understanding the circumstances and consequences of the fall, along with past fall history and relevant medical conditions, informs risk stratification and intervention planning. Specific indicators, such as injury severity, recurrent falls, prolonged inability to get up, frailty, and suspected loss of consciousness, are strong predictors of future falls risk and warrant immediate attention and comprehensive assessment.
Assessment and Algorithm Flow: Streamlining Risk Stratification
The proposed algorithm (Figure 1) offers two entry points for falls risk stratification: opportunistic case-finding during routine health visits or through electronic health records, and presentation to healthcare services following a fall or related injury. Opportunistic case-finding is essential as many older adults do not spontaneously report falls or seek medical attention after a fall event. Furthermore, recall of previous falls, particularly the exact timing, can be unreliable. The 12-month timeframe for fall history inquiry represents a pragmatic balance between recall accuracy and the typical progression of falls risk factors.
Initial opportunistic case-finding can begin with the simple question: “Have you fallen in the last 12 months?” This question exhibits high specificity in predicting future falls but may have lower sensitivity, potentially missing individuals with significant risk factors who have not yet experienced a fall. Tools like the “three key questions” (3KQ) enhance sensitivity by incorporating additional risk indicators: (i) Have you fallen in the past year? (ii) Do you feel unsteady when standing or walking? (iii) Do you worry about falling? The Stay Independent self-risk assessment, part of the CDC’s STEADI toolkit, is another sensitive approach for detecting future fall risk, comprising 12 self-administered questions. The sensitivity of falls risk screening tools, including the single-question approach, varies with age, increasing with advancing age. Gait or balance disturbances should be assessed following a positive response to fall history or any of the 3KQ.
Strong Recommendation. For objective gait and balance assessment, gait speed measurement is recommended for predicting falls risk. GRADE: 1A. The Timed Up and Go (TUG) test can be considered as an alternative, although its evidence base for fall prediction is less consistent. GRADE: 1B.
Recommendation Details and Justification
Gait speed is a robust and widely validated predictor of falls risk in older adults, reflecting overall physical function and mobility. The TUG test provides a comprehensive measure of mobility, incorporating вставание from a chair, walking, and turning, but its predictive validity for falls is less consistently demonstrated compared to gait speed. Both tests are easily administered in clinical settings and offer valuable objective data for falls risk stratification.
Based on the algorithm, older adults are categorized into low, intermediate, or high risk. Individuals with no fall history or a single non-severe fall and no gait/balance problems are considered low risk. However, low risk does not equate to no risk, and primary prevention strategies, including annual reassessment, are recommended. Older adults with a single non-severe fall and gait/balance issues are classified as intermediate risk and benefit from strength and balance exercise interventions, which have proven effective in reducing falls risk. High-risk individuals include those with a fall accompanied by injury, recurrent falls (≥2 in 12 months), known frailty, inability to get up after a fall for at least an hour, or suspected transient loss of consciousness. These individuals require a multifactorial falls risk assessment to guide tailored interventions. Suspected syncopal falls warrant syncope evaluation and management. Frailty assessment, whether previously identified or detected using validated instruments like the Frailty Phenotype (FP) or Clinical Frailty Scale (CFS), is a critical component of risk stratification. The FP encompasses five criteria (slow gait speed, low physical activity, unintentional weight loss, exhaustion, and muscle weakness), while the CFS is a semi-quantitative scale ranging from very fit to terminally ill. A CFS score of ≥4 indicates frailty. The algorithm (Figure 1) provides a visual summary of this risk stratification and management approach.
Comprehensive Falls Risk Assessment: Identifying Modifiable Risk Factors
The primary objectives of a comprehensive falls risk assessment are to elucidate the mechanism of falls, evaluate the consequences (injuries, functional deficits, psychological impact like fear of falling), and identify contributing fall risk factors. A thorough assessment considers the older adult’s fall history (frequency, characteristics, context), the presence of risk factors, physical, cognitive, psychological, and social resources, and their individual goals, values, beliefs, and priorities. A person-centered approach, exemplified by a comprehensive geriatric assessment (CGA), is essential for co-designing effective interventions. The 2019 World Falls Guidelines’ recommendations, based on evidence-based WG reviews, outline the necessary assessments to identify key modifiable falls risk factors. Table 4 provides an overview of potential measurement instruments and approaches for assessing individual modifiable risk factors across various domains.
Table 4. Measurement Instruments and Approaches for Multifactorial Falls Risk Assessment
| Domain for Assessment | Fall Risk Factor | Measurement/Approach |
|---|---|---|
| Mobility | Balance | Screen for balance disorders (e.g., Tandem Stand, One Leg Stand). If indicated, conduct full assessment (e.g., Berg Balance Scale, Tinetti test, POMA balance subscale, Mini-BEST test). Consider physiotherapy referral. |
| Gait | Assess gait qualitatively and quantitatively using 4-meter walk test. Screen for mobility problems using structured approaches (e.g., SPPB, TUG, Get Up and Go with qualitative assessment). | |
| Muscle strength | Screen quantitatively using CST or handgrip strength. If indicated, assess specific muscle groups structurally (MRC scale). | |
| Walking aid | If applicable, assess appropriateness and proper use of walking aids, including mechanical condition. | |
| Footwear and foot problems | Screen for inappropriate footwear (including barefoot walking). Assess for foot problems. Consider podiatrist referral. | |
| Fear of falling | Assess fear of falling using structured instruments (e.g., FES-I, short FES-I). If indicated, assess for anxiety disorders (e.g., HADS). Consider specialist referral. | |
| Sensory function | Dizziness/vestibular | Screen with history taking and Dix-Hallpike/Head Impulse Test if indicated. Consider ENT/ORL specialist referral. |
| Vision | Assess subjective vision problems (history taking). Objective assessment of visual acuity and problems, proper glasses use (including multi/bifocal check). Refer to ophthalmologist/optometrist if indicated. | |
| Hearing | Assess subjective hearing problems (history taking). Objective hearing assessment. Refer to audiologist/ENT/ORL specialist if indicated. | |
| Activities of daily living | Functional ability | Assess ADL and IADL using structured tools (e.g., modified Katz for community dwellers, NEADL or Barthel for personal care/care home residents). |
| Cognitive function | Cognition | Screen for cognitive disorders, including executive function (e.g., Clock Drawing Test, MoCA, TMT-B). Further assessment and neuropsychological testing if indicated. |
| Delirium | Assess for delirium using structured tools (e.g., 4AT, DOS, CAM) and clinical judgment. | |
| Behavior | Assess behavior, preferably using structured methods. | |
| Autonomic function | Orthostatic Hypotension | Measure blood pressure supine (after 5 min rest) and upon standing (repeatedly at intervals up to 3-5 min). Check for symptom recognition. |
| Urinary incontinence | Assess with 3IQ screening test. Additional testing and/or urologist/gynecologist referral. | |
| Disease history | Cardiovascular disorders | Assess with focused history (cardiovascular symptoms, history), physical exam, orthostatic BP, ECG. Further assessment (tilt table testing, rhythm/BP monitoring) if indicated. Cardiologist/syncope specialist referral. |
| Contributing diseases/atypical presentation | Clinical geriatric assessment (history, physical exam, labs, additional testing) focusing on diabetes, osteoarthritis, neurological disorders (PD, polyneuropathy, stroke), cardiovascular diseases, cognition, depression, delirium, anemia, electrolyte disorders, thyroid disease, frailty, sarcopenia, fracture risk. Assess for atypical presentation of acute conditions (e.g., pneumonia). | |
| Parkinson Disease | Assess mobility (gait, balance, strength, FOG), cognition (dual tasking), orthostatic hypotension. | |
| Depressive disorders | Screen for depression (e.g., GDS, 2-question screen). Specialist referral if indicated. | |
| Medication history | Medication | Structured medication review, considering deprescribing FRIDs (e.g., STOPPFall, STEADI instrument). |
| Nutrition history | Nutritional status | Screen for malnutrition (e.g., MNA, MUST, MST), obesity, sarcopenia, vitamin deficiencies (D, B1, B12, folate), substance abuse, alcohol use. |
| Vitamin D | Assess vitamin D status based on local guidelines. Supplementation standard for high-risk groups (care home residents, homebound). | |
| Environmental risk | Environment | Recommended hazard assessment tools: Westmead Home Safety Assessment, Falls Behavioural Scale for Older Person. LMIC: self-administered checklists available. |
Table 5. Recommendations from the 2019 World Falls Guidelines by Working Groups
| WG/Domains | Area or Domain | Recommendation | Grade |
|---|---|---|---|
| WG 1 Gait and Balance Assessment Tools to Assess Risk for Falls | Stratification | Recommend gait speed for falls risk prediction. TUG test as alternative, but less consistent evidence. | 1A/1B |
| Assessment | Recommend gait and balance assessment. | 1B | |
| WG 2 Polypharmacy, Fall Risk Increasing Drugs, and Falls | Assessment | Recommend assessing fall history and risk before prescribing FRIDs to older adults. | 1B |
| Assessment | Recommend validated screening/assessment tool for FRIDs in medication review for falls prevention. | 1C | |
| Intervention | Recommend medication review and FRID deprescribing as part of multidomain falls prevention. | 1B | |
| Intervention | Recommend rational deprescribing of FRIDs in falls prevention for long-term care residents. | 1C | |
| WG 3 Cardiovascular Risk Factors for Falls | Assessment | Recommend cardiovascular assessment (history, auscultation, orthostatic BP, ECG) as part of multifactorial assessment. | 1B |
| Assessment | No further cardiovascular assessment needed if initial assessment normal, unless syncope suspected. | 1C | |
| Assessment | Recommend further cardiovascular assessment for unexplained falls same as for syncope, in addition to multifactorial assessment. | 1A | |
| Intervention | Recommend orthostatic hypotension management as part of multidomain intervention for fallers. | 1A | |
| Intervention | Recommend interventions for cardiovascular disorders identified during falls risk assessment same as for syncope-associated conditions, in addition to other multifactorial interventions. | 1B | |
| WG 4 Exercise Interventions for Prevention of Falls and Related Injuries | Exercise Intervention | Recommend exercise programs for community-dwelling older adults including balance challenging and functional exercises (e.g., sit-to-stand, stepping), ≥3 sessions/week, individualized, progressed intensity, ≥12 weeks, continued longer for greater effect. | 1A |
| Exercise Intervention | Recommend inclusion of Tai Chi and/or progressive resistance strength training when feasible. | 1B | |
| Exercise Intervention | Recommend individualized supervised exercise for falls prevention in long-term care settings. | 1B | |
| Exercise Intervention | Recommend individualized exercise programs including balance and resistance training for adults with early-mid stage PD and mild/no cognitive impairment. | 1A | |
| Exercise Intervention | Conditionally recommend individualized exercise for balance/strength/walking improvement to prevent falls in adults post-stroke. | 2C | |
| Exercise Intervention | Recommend individualized progressive exercise to improve mobility (standing, balance, walking, stairs) as falls prevention for adults post-hip fracture. | 1B | |
| Exercise Intervention | Conditionally recommend post-hip fracture programs start inpatient and continue in community. | 2C (Inpatient) & 1A (Community) | |
| Intervention | Recommend exercise for falls prevention for community-dwelling adults with cognitive impairment (MCI, mild-moderate dementia) if willing and able. | 1B | |
| WG 5 Falls in Hospitals and Care Homes | Hospital Assessment | Recommend multifactorial falls risk assessment for hospitalized older adults >65 years. Recommend against scored falls risk screening tools in hospitals. | 2B |
| Hospitals management and interventions | Recommend tailored falls prevention education for all hospitalized older adults (≥65 years) and high-risk groups. | 1A | |
| Hospitals management and interventions | Recommend personalized single/multidomain falls prevention strategies based on risk factors/behaviors for all hospitalized older adults (≥65 years) or younger at-risk individuals identified by professionals. | 1C (Acute care) & 1B (Sub-acute care) | |
| Care homes assessment | Recommend against falls risk screening to identify at-risk care home residents. All residents considered high risk. | 1A | |
| Care homes assessment | Recommend multifactorial falls risk assessment at admission to identify risk factors and implement interventions in care home residents. | 1C | |
| Care homes assessment | Recommend post-fall assessment in care home residents to reassess risk factors, adjust intervention, avoid unnecessary acute care transfer. | E |
(Continued)
Table 5. Continued Recommendations from the 2019 World Falls Guidelines by Working Groups
| WG/Domains | Area or Domain | Recommendation | Grade |
|---|---|---|---|
| Care Homes Management and Interventions | Recommend multifaceted approach for falls reduction in care homes: staff training, multidomain decision support tool, falls prevention actions. | 1B | |
| Recommend against physical restraints for falls prevention in care homes. | 1B | ||
| Recommend nutritional optimization (calcium/protein-rich food, vitamin D supplementation) as part of multidomain intervention for care home residents. | 1B | ||
| Recommend promotion of physical activity (when feasible/safe) as part of multidomain falls prevention in care homes. | 1C | ||
| WG 6 Cognition and Falls | Cognition Assessment | Recommend routine cognition assessment as part of multifactorial falls risk assessment in older adults. | 1B |
| Cognition Assessment | Recommend including older adult’s and caregiver’s perspectives in falls prevention care plans for adults with cognitive impairment for better adherence/outcomes. | 1C | |
| WG 7 Falls and PD and Related Disorders | Assessment | Conditionally recommend falls risk assessment for older adults with PD, including self-report 3-risk factor tool (fall history, FOG, slow gait speed). | 2B |
| Management and Intervention | Conditionally recommend multidomain interventions for older adults with PD. | 2B | |
| Management and Intervention | Recommend individualized exercise programs (balance/resistance training) for adults with early-mid stage PD and mild/no cognitive impairment. | 1A | |
| Management and Intervention | Conditionally recommend exercise training (balance/strength) for people with complex phase PD if supervised by qualified professional. | 1C | |
| WG 8 Falls and Technology | Assessment and Interventions | Conditionally recommend telehealth/smart home systems (when available) with physical exercise as part of community falls prevention. | 2C |
| Interventions | Current evidence does not support wearables for falls prevention. Emerging evidence shows wearables in exercise programs may increase participation. | 2C | |
| WG 9 Falls in Low- and Middle-Income Countries | Implementation | Local context needs consideration when implementing falls prevention in LMIC. | 1B |
| Assessment | Conditionally recommend prioritizing assessments of cognitive impairment, obesity (sarcopenic obesity), diabetes, inappropriate footwear, environmental hazards as falls risk factors in LMIC. | 2C | |
| Assessment | Conditionally recommend validated, freely available tools in LMIC to assess mobility, dependent on resource availability. | E | |
| WG 10 Multifactorial Assessment and Interventions for Falls (Environment informed by ad hoc expert group) | Multifactorial Assessment | Recommend multiprofessional, multifactorial assessment for high-risk community-dwelling older adults to guide tailored interventions. | 1B |
| Multidomain Interventions | Recommend multidomain interventions, informed by multiprofessional, multifactorial assessment, for high-risk community-dwelling older adults. | 1B | |
| Multifactorial (Environmental) Assessment | Recommend clinician-led identification of environmental hazards in individual’s home and assessment of capacities/behaviors in relation to hazards as part of multifactorial assessment. | 1B | |
| Multifactorial (Environmental) Interventions | Recommend modifications of home environment for fall hazards by trained clinician, considering capacities/behaviors, as part of multidomain intervention. | 1B | |
| WG 11 Older Adults’ Perspectives on Falls | Stratification | Recommend clinicians routinely ask about falls in interactions with older adults. | 1A |
| Assessment | Recommend clinicians inquire about older adult’s perceptions of falls, causes, risk, and prevention as part of comprehensive assessment. | 1B | |
| Interventions | Recommend care plan to prevent falls/injuries incorporate goals, values, preferences of older adult. | 1B | |
| WG 12 Concerns about Falling and Falls | Assessment | Recommend evaluating concern about falling in multifactorial falls risk assessment. | 1B |
| Assessment | Recommend standardized instrument (FES-I, Short FES-I) to evaluate concerns about falling in community-dwelling older adults. | 1A | |
| Assessment | Recommend FES-I or Short FES-I for assessing concerns about falling in acute care/long-term care. | 1B | |
| Assessment | Recommend exercise, CBT, and/or occupational therapy (multidisciplinary approach) to reduce fear of falling in community-dwelling older adults. | 1B |
Note: These are the 12 original Working Groups that addressed knowledge gaps identified from review of previous clinical practice guidelines.
While a CGA encompasses broader geriatric syndromes, the 2019 WFG focuses on falls risk factors directly. However, it acknowledges the significant associations between falls and other geriatric syndromes, emphasizing that falls, especially in frail older adults, can be a sentinel event indicating underlying conditions. Falls may be the presenting symptom of acute medical conditions like pneumonia (particularly with delirium) or myocardial infarction without chest pain. Therefore, assessment choices should consider the older adult’s clinical profile (frail vs. non-frail), care setting (community, clinic, acute care, long-term care), and available resources (cost, training, equipment).
Incorporating the Older Adult’s Perspective: Person-Centered Care
Strong Recommendation. As part of a multifactorial falls risk assessment, clinicians should inquire about the older adult’s perceptions of falls, their perceived causes, future risk, and prevention strategies. GRADE: 1B.
Expert Recommendation. Clinicians should also inquire about the older adult’s goals and priorities, attitudes towards activity, independence, and risk, and their willingness and capacity to actively participate in decision-making regarding potential interventions. GRADE: E.
Recommendation Details and Justification
Integrating the older adult’s perspective is central to person-centered falls prevention. Understanding their beliefs about falls, their perceived risk, and their priorities for intervention enhances engagement and adherence. Exploring their attitudes towards activity, independence, and risk tolerance helps tailor interventions that align with their values and preferences. Shared decision-making empowers older adults to actively participate in their care, leading to more effective and sustainable prevention strategies.
Multifactorial Falls Risk Assessment: Core Domains
Strong Recommendation. Offer multiprofessional, multifactorial assessment to community-dwelling older adults identified as high risk to guide tailored interventions. GRADE: 1B.
Recommendation Details and Justification
A multifactorial falls risk assessment for high-risk individuals encompasses a comprehensive evaluation across multiple domains to inform personalized falls prevention and management interventions. These domains include:
- Gait and balance: Assessing stability and mobility.
- Muscle strength: Evaluating lower limb and overall strength.
- Medications: Reviewing medications, particularly fall-risk increasing drugs (FRIDs).
- Cardiovascular disorders: Assessing for orthostatic hypotension and cardiac conditions.
- Dizziness: Investigating vestibular and cardiovascular causes.
- Functional ability and walking aids: Evaluating ADLs and proper use of assistive devices.
- Vision and hearing: Assessing sensory impairments.
- Musculoskeletal disorders: Identifying arthritis and other musculoskeletal conditions.
- Foot problems and footwear: Evaluating foot health and shoe appropriateness.
- Neurocognitive disorders: Assessing for delirium, dementia, and cognitive impairment.
- Neurological disorders: Identifying Parkinson’s disease, neuropathy, and stroke.
- Underlying diseases: Considering acute and chronic medical conditions.
- Concerns about falling: Assessing fear of falling and its impact on activity.
- Environmental hazards: Evaluating home safety and environmental risks.
- Nutritional status: Assessing for malnutrition and vitamin D deficiency.
- Alcohol consumption: Evaluating alcohol intake and its potential contribution to falls.
- Urinary incontinence: Assessing bladder control issues.
- Pain: Evaluating pain levels and their impact on mobility and falls risk.
The evidence supporting multifactorial assessment stems from the effectiveness of multidomain interventions that are tailored to address individual risk factors identified through comprehensive assessment. This approach contrasts with generic interventions applied indiscriminately, highlighting the importance of personalized care in falls prevention. The strength of evidence varies across individual components, with detailed information provided in subsequent sections.
Assessment Details for Individual Components: Domain-Specific Evaluations
Gait and Balance Assessment: Evaluating Mobility and Stability
Strong Recommendation. Gait and balance should be assessed as part of falls risk assessment. GRADE: 1B.
Recommendation Details and Justification
Gait and balance impairments are major risk factors for falls. Objective assessment using validated tools is crucial for identifying deficits and guiding targeted interventions, such as balance and strength training.
Medication Assessment: Identifying and Managing Fall-Risk Increasing Drugs (FRIDs)
Strong Recommendation. Assess for fall history and falls risk before prescribing potential FRIDs to older adults. GRADE: 1B.
Strong Recommendation. Use a validated, structured screening and assessment tool to identify FRIDs during medication reviews for falls prevention. GRADE: 1C.
Recommendation Details and Justification
Medications, particularly FRIDs, significantly contribute to falls risk. Routine medication review, especially when initiating new FRIDs or in individuals with fall history, is essential. Structured tools aid in identifying FRIDs and guiding deprescribing strategies to minimize medication-related falls risk.
Cognitive Assessment: Evaluating Cognitive Function and its Impact on Falls
Strong Recommendation. Cognition assessment should be included in multifactorial falls risk assessment. GRADE: 1B.
Recommendation Details and Justification
Cognitive impairment, including dementia and executive dysfunction, is an independent falls risk factor. Cognitive assessment helps identify individuals who may benefit from tailored interventions, such as dual-task training and environmental modifications, to mitigate cognitive-related falls risk.
Concerns about Falling: Addressing Fear of Falling and Activity Restriction
Strong Recommendation. Evaluate concerns about falling in multifactorial falls risk assessment. GRADE: 1B.
Strong Recommendation. Use standardized instruments like FES-I or Short FES-I to evaluate concerns about falling in community-dwelling older adults. GRADE: 1A.
Recommendation Details and Justification
Fear of falling is a significant consequence of falls and can lead to activity restriction, social isolation, and further functional decline. Routine assessment of fear of falling using validated tools like FES-I is crucial for identifying individuals who may benefit from interventions such as exercise, cognitive behavioral therapy, or occupational therapy to reduce fear and improve activity levels.
Cardiovascular Assessment: Identifying and Managing Cardiovascular Risk Factors
Strong Recommendation. Perform cardiovascular assessment (cardiac history, auscultation, orthostatic BP, 12-lead ECG) as part of multifactorial falls risk assessment. GRADE: 1B.
Strong Recommendation. No further cardiovascular assessment needed if initial assessment is normal, unless syncope is suspected. GRADE: 1C.
Strong Recommendation. Further cardiovascular assessment for unexplained falls should be same as for syncope, in addition to multifactorial falls risk assessment. GRADE: 1A.
Recommendation Details and Justification
Cardiovascular conditions, particularly orthostatic hypotension and arrhythmias, are significant falls risk factors. Routine cardiovascular assessment helps identify these conditions and guide appropriate medical management as part of a comprehensive falls prevention strategy. Syncope suspicion warrants further specialized cardiovascular evaluation.
Dizziness and Vestibular Disorders Assessment: Investigating Vestibular Contributions to Falls
Expert Recommendation. Routinely ask about dizziness symptoms and undertake follow-up assessment to identify cardiovascular, neurological, and/or vestibular causes. GRADE: E.
Recommendation Details and Justification
Dizziness is a common complaint among older adults who fall, often with multifactorial etiologies. Careful history taking and targeted vestibular assessments, such as Dix-Hallpike and Head Impulse tests, are crucial for identifying vestibular dysfunction, a treatable cause of falls. Vestibular rehabilitation can effectively improve balance and reduce falls risk in individuals with vestibular disorders.
Vision and Hearing Assessment: Addressing Sensory Impairments
Expert Recommendation. Enquire about vision impairment as part of multifactorial falls risk assessment, measure visual acuity, and examine for other visual impairments. GRADE: E.
Expert Recommendation. Enquire about hearing impairment as part of multifactorial falls risk assessment, measure and examine for hearing impairments, and refer to specialist if appropriate. GRADE: E.
Recommendation Details and Justification
Vision and hearing impairments are independent falls risk factors. Routine assessment of visual acuity, contrast sensitivity, depth perception, and hearing function is essential. Corrective measures, such as updated glasses prescriptions and hearing aids, can significantly reduce falls risk associated with sensory deficits. Accessibility to vision and hearing assessments should be emphasized, particularly in LMICs.
Delirium: Recognizing and Managing Delirium-Related Falls
Delirium, cognitive impairment, and dementia are independent risk factors for falls across various care settings. Effective management of these conditions is crucial for falls prevention. Environmental adaptations and caregiver education on safe mobility strategies are beneficial for older adults with delirium. Staff education on delirium management can also reduce falls in hospitalized older adults. Multidomain strategies to prevent delirium, including cognitive stimulation, orientation, early mobilization, vision and hearing optimization, and family involvement, should be considered as part of comprehensive care packages for hospitalized older adults. Balancing mobility promotion with falls prevention is crucial, especially in frail older adults.
Urinary Symptoms and Incontinence Assessment: Addressing Continence-Related Falls Risk
Expert Recommendation. Enquire about urinary symptoms as part of multifactorial falls risk assessment. GRADE: E.
Recommendation Details and Justification
Urinary incontinence and nocturia are associated with increased falls risk, particularly during nighttime trips to the bathroom. Assessment of urinary symptoms helps identify individuals who may benefit from continence management strategies, such as bladder training, pelvic floor exercises, and environmental modifications like nightlights and bedside commodes.
Pain Assessment: Managing Pain to Improve Mobility and Reduce Falls
Expert Recommendation. Enquire about pain as part of multifactorial falls risk assessment, followed by comprehensive pain assessment if indicated. GRADE: E.
Recommendation Details and Justification
Pain, particularly chronic pain, can impair mobility, balance, and gait, increasing falls risk. Routine pain assessment and effective pain management strategies, including pharmacological and non-pharmacological approaches, are crucial for improving function and reducing falls risk in older adults with pain.
Environmental Assessment: Identifying and Modifying Home Hazards
Strong Recommendation. Clinician-led identification of environmental hazards in an individual’s home and assessment of their capacities and behaviors in relation to hazards should be part of multifactorial falls risk assessment. GRADE:1B.
Recommendation Details and Justification
Environmental hazards in the home significantly contribute to falls risk. Assessment by trained clinicians, such as occupational therapists, should evaluate home hazards, individual capacities, and behaviors in relation to these hazards. Tools like the Westmead Home Safety Assessment and Falls Behavioural Scale for the Older Person are recommended for comprehensive environmental risk assessment. Addressing environmental hazards through modifications and assistive devices is a key component of multidomain falls prevention interventions. In LMICs, training personnel for environmental assessments and providing affordable equipment are crucial.
Depression Assessment: Addressing Mental Health and Falls Risk
Expert Recommendation. Enquire about depressive symptoms as part of multifactorial falls risk assessment, followed by further mental state assessment and specialist referral if necessary. GRADE: E.
Recommendation Details and Justification
Depression is associated with increased falls risk, potentially due to factors like psychomotor slowing, medication side effects, and reduced motivation for physical activity. Routine screening for depressive symptoms and appropriate mental health management are important components of a comprehensive falls prevention approach.
Nutritional Assessment including Vitamin D: Optimizing Nutrition for Bone and Muscle Health
Expert Recommendation. Assess nutritional status including vitamin D intake as part of multifactorial falls risk assessment, followed by supplementation where appropriate. GRADE: E.
Recommendation Details and Justification
Nutritional deficiencies, including vitamin D insufficiency and malnutrition, can contribute to muscle weakness, bone fragility, and increased falls risk. Nutritional assessment, including vitamin D status, and appropriate nutritional interventions, such as vitamin D supplementation and protein optimization, are important for maintaining musculoskeletal health and reducing falls risk.
Assessment of Fracture Risk: Integrating Bone Health Management
While not explicitly detailed within the falls prevention guidelines, assessment of fracture risk and integration with bone health management services are crucial complements to falls prevention. Close clinical and epidemiological links between falls and fragility fractures necessitate explicit coordination with clinicians and services specializing in osteoporosis and fracture risk management.
Management and Interventions: Strategies for Falls Prevention
Management of Older Adults at Low Fall Risk: Promoting Safe Mobility and Healthy Lifestyle
Expert Recommendation. Provide advice on maintaining safe mobility and optimizing physical functioning to older adults at low falls risk from a trained clinician. Advice should consider individual circumstances, priorities, preferences, and resources, reinforcing health promotion/prevention messaging relevant to falls and fracture risks (physical activity, lifestyle habits, nutrition including vitamin D intake). GRADE: E.
Recommendation Details and Justification
Low falls risk does not mean no risk. Primary prevention strategies for low-risk older adults focus on promoting healthy lifestyles and safe mobility practices. This includes advice on regular physical activity, balance exercises, healthy nutrition, and home safety. Referral to community-based health promotion or “aging well” programs may be beneficial. Fracture risk management, including osteoporosis screening and treatment, should also be addressed. Generic health promotion guidelines from organizations like WHO and national health bodies offer valuable resources for low-risk falls prevention advice.
Interventions for Community-Dwelling Older Adults at Intermediate Fall Risk: Targeted Exercise Programs
Expert Recommendation. Offer an exercise program based on individual assessment and recommendations in the Exercise Interventions section. GRADE: E.
Recommendation Details and Justification
Supervised exercise programs targeting balance and strength are effective in preventing falls in intermediate-risk older adults. Exercise should focus on functional tasks relevant to daily life, such as sit-to-stand, walking, and stair climbing. Individualized exercise plans, progressed in intensity and complexity, are crucial for achieving optimal falls prevention benefits.
Multidomain Interventions for Community-Dwelling Older Adults at High Fall Risk: Person-Centered, Comprehensive Approach
Developing a Person-Centered Intervention: Shared Decision-Making and Individualized Care
A person-centered falls prevention plan for high-risk older adults is based on a holistic multifactorial falls risk assessment and shared decision-making. This approach prioritizes the older adult’s goals, preferences, beliefs, and resources, along with relevant caregiver input. The intervention plan should address individually relevant risk factors within the context of other geriatric syndromes and conditions.
Strong Recommendation. A care plan to prevent falls and injuries should incorporate the values and preferences of the older adult. GRADE: 1B.
Strong Recommendation. When creating falls prevention care plans for older adults with cognitive impairment, include both older adults’ and caregivers’ perspectives for improved adherence and outcomes. GRADE: 1C.
Recommendation Details and Justification
Engaging older adults in shared decision-making enhances adherence and outcomes. Understanding their perspectives on falls, perceived risk, and intervention preferences is crucial. For individuals with cognitive or functional limitations, caregiver involvement and training are essential for successful intervention implementation. Falls prevention interventions can be intensive and long-term, requiring informed consent and realistic expectations regarding benefits and burdens.
Multidomain Falls Risk Intervention: Comprehensive and Tailored Strategies
Strong Recommendation. Offer multidomain interventions, informed by a multiprofessional, multifactorial falls risk assessment, to high-risk community-dwelling older adults. GRADE: 1B.
Recommendation Details and Justification
Multidomain interventions are the cornerstone of falls prevention for high-risk older adults. These interventions combine two or more components, tailored to the individual based on their multifactorial falls risk assessment. A multidomain intervention typically includes:
- Strength and balance exercise: Targeted exercise programs to improve mobility and stability.
- Medication review: Deprescribing FRIDs and optimizing medication regimens.
- Management of orthostatic hypotension and cardiovascular diseases: Addressing cardiovascular risk factors for falls.
- Management of underlying acute and chronic diseases: Treating medical conditions contributing to falls risk.
- Vision and hearing optimization: Correcting sensory impairments.
- Foot care and appropriate footwear: Addressing foot problems and footwear issues.
- Vitamin D supplementation: Supplementation for individuals at risk of deficiency.
- Nutritional optimization: Ensuring adequate nutrition, including protein intake.
- Continence management: Addressing urinary incontinence.
- Interventions to address concerns about falling: Reducing fear of falling and activity restriction.
- Individual education: Providing falls prevention education and self-management strategies.
- Environmental modification: Home safety assessments and modifications.
These components are derived from robust systematic reviews and meta-analyses demonstrating the effectiveness of multidomain interventions in reducing falls. However, pragmatic RCTs in real-world settings highlight the importance of adequate resources and fidelity in intervention delivery to achieve optimal outcomes.
Component Interventions: Evidence-Based Strategies for Falls Prevention
Exercise and Physical Activity Interventions: Enhancing Balance and Strength
Strong Recommendation. Exercise programs for community-dwelling older adults should include balance-challenging and functional exercises (e.g., sit-to-stand, stepping), ≥3 sessions/week, individualized, progressed intensity, ≥12 weeks, and continued longer for greater effect. GRADE: 1A.
Strong Recommendation. Include Tai Chi and/or progressive resistance strength training when feasible. GRADE: 1B.
Recommendation Details and Justification
Exercise is a cornerstone of falls prevention. Balance training, functional exercises, Tai Chi, and progressive resistance training have all demonstrated effectiveness in reducing falls risk. Exercise programs should be individualized, progressive, and sustained to achieve optimal benefits.
Medication Interventions: Medication Review and Deprescribing FRIDs
Strong Recommendation. Medication review and appropriate deprescribing of FRIDs should be part of multidomain falls prevention interventions. GRADE: 1B.
Strong Recommendation. Rational deprescribing of FRIDs should always be included in falls prevention strategies for long-term care residents. GRADE: 1C.
Recommendation Details and Justification
Medication review and deprescribing of FRIDs are essential components of multidomain falls prevention. Structured medication reviews, guided by validated tools, help identify and deprescribe unnecessary or high-risk medications, reducing medication-related falls risk.
Cardiovascular Interventions: Managing Orthostatic Hypotension and Cardiovascular Conditions
Strong Recommendation. Management of orthostatic hypotension should be included in multidomain interventions. GRADE: 1A.
Strong Recommendation. Interventions for cardiovascular disorders identified during falls risk assessment should be the same as for syncope-associated conditions, in addition to other multifactorial interventions. GRADE 1B.
Recommendation Details and Justification
Managing orthostatic hypotension and underlying cardiovascular conditions is crucial for falls prevention. Strategies include medication adjustments, rehydration, compression garments, and medications for orthostatic hypotension. Management of syncope and cardiovascular disorders should align with local syncope guidelines.
Telehealth and Technology Interventions: Leveraging Digital Tools for Falls Prevention
Expert Recommendation. Use telehealth and/or smart home systems (when available) in combination with exercise training as part of community falls prevention programs. GRADE: E.
Conditional Recommendation. Current evidence does not support wearables for falls prevention. However, emerging evidence shows wearables in exercise programs may increase participation. GRADE: 2C.
Recommendation Details and Justification
Telehealth and smart home technologies offer promising avenues for delivering and enhancing falls prevention interventions, particularly in community settings. Telehealth can facilitate remote exercise programs and monitoring, while smart home systems can detect falls and reduce environmental hazards. Wearables may enhance exercise program adherence, but their direct impact on falls prevention remains under investigation.
Environmental Interventions: Modifying Home Hazards for Safer Environments
Strong Recommendation. Recommendations for home environment modifications to address fall hazards, considering individual capacities and behaviors, should be provided by a trained clinician as part of multidomain falls prevention. GRADE: 1B.
Recommendation Details and Justification
Home modifications to address environmental hazards, guided by trained professionals, are effective in reducing falls risk. Modifications should be tailored to individual needs, capacities, and behaviors within their home environment.
Vestibular Interventions: Managing Vestibular Dysfunction for Balance Improvement
Expert Recommendation. Managing vestibular issues should be considered as part of a multifactorial approach. GRADE: E
Recommendation Details and Justification
Vestibular rehabilitation, including particle repositioning maneuvers (Epley) for benign paroxysmal positional vertigo, can effectively improve balance and reduce falls risk in individuals with vestibular dysfunction. These interventions are low-cost and can be implemented in resource-limited settings.
Pain Interventions: Optimizing Pain Management for Improved Function
Expert Recommendation. Adequate pain treatment should be considered as part of the multidomain approach. GRADE: E.
Recommendation Details and Justification
Effective pain management improves mobility, function, and quality of life, indirectly reducing falls risk associated with pain-related limitations. Pain management strategies should be integrated into multidomain falls prevention plans for individuals with pain.
Concerns about Falling Interventions: Reducing Fear and Restoring Activity
Strong Recommendation. Recommend exercise, cognitive behavioral therapy, and/or occupational therapy (multidisciplinary approach) to reduce concerns about falling in community-dwelling older adults. GRADE: 1B.
Recommendation Details and Justification
Exercise, cognitive behavioral therapy (CBT), and occupational therapy are effective in reducing fear of falling and improving activity levels. These interventions should be considered as part of a multidisciplinary approach to address fear of falling in older adults. Supervised holistic exercise interventions like Pilates and yoga may be particularly beneficial in reducing fear of falling.
Vision Interventions: Optimizing Vision for Enhanced Environmental Awareness
Expert Recommendation. Management of impaired vision should be considered as part of the multifactorial approach. GRADE: E.
Recommendation Details and Justification
Vision correction, cataract surgery, and management of other vision impairments are crucial for reducing falls risk associated with visual deficits. Vision interventions should be integrated into multidomain falls prevention plans.
Vitamin D Interventions: Targeted Supplementation for Vitamin D Deficiency
If older adults are at risk of vitamin D deficiency, daily vitamin D supplementation should be recommended per national guidelines. However, universal vitamin D supplementation for falls prevention is not supported by current evidence. Vitamin D supplementation is most likely to benefit individuals with frank vitamin D deficiency, such as frail older adults and care home residents. Targeted vitamin D supplementation, guided by risk assessment and vitamin D level testing, is recommended.
Falls in Hospitals: Prevention in the Acute Care Setting
Risk Stratification and Assessment in Hospitals: Tailoring Assessment to the Hospital Environment
Conditional Recommendation. Perform multifactorial falls risk assessment in all hospitalized older adults >65 years of age. Recommend against using scored falls risk screening tools in hospitals for multifactorial falls risk assessment. GRADE: 2B.
Strong Recommendation. Recommend FES-I or Short FES-I for assessing concerns about falling in acute care hospitals. GRADE: 1B.
Expert Recommendation. Recommend post-fall assessment in hospitalized older adults to identify fall mechanism, injuries, precipitating factors (illness, delirium), reassess risk factors, and adjust intervention strategy. GRADE: E.
Recommendation Details and Justification
Multifactorial falls risk assessment is essential for hospitalized older adults. Scored falls risk screening tools are not recommended in hospitals as they do not effectively reduce falls and may divert resources from more comprehensive assessment and intervention strategies. Post-fall assessments are crucial for understanding fall events in hospitals and guiding individualized prevention strategies. Assessing fear of falling using FES-I or Short FES-I is also recommended in the acute care setting.
Management and Interventions in Hospitals: Implementing Tailored Prevention Strategies
Strong Recommendation. Tailored falls prevention education should be delivered to all hospitalized older adults (≥65 years) and other high-risk groups. GRADE: 1A.
Strong Recommendation. Personalized single or multidomain falls prevention strategies based on identified risk factors, behaviors, or situations should be implemented for all hospitalized older adults (≥65 years) or younger at-risk individuals identified by health professionals. GRADE: 1C (Acute care), GRADE: 1B (Sub-acute care).
Recommendation Details and Justification
Falls prevention in hospitals requires a multifaceted approach including education and personalized interventions. Tailored education for patients and staff is crucial. Personalized interventions, based on multifactorial assessment, should address individual risk factors and be implemented across acute and sub-acute care settings.
Falls in Care Homes: Prevention in Long-Term Care Facilities
Risk Stratification and Assessment in Care Homes: Universal High-Risk Approach
Strong Recommendation. Do not perform falls risk screening to identify at-risk care home residents as all residents should be considered high risk. GRADE: 1A.
Strong Recommendation. Perform comprehensive multifactorial assessment at admission to identify risk factors and implement appropriate interventions in care home older adults. GRADE: 1C.
Expert Recommendation. Recommend post-fall assessment in care home residents to identify fall mechanism, injuries, reassess resident’s risk factors, adjust intervention, and avoid unnecessary hospital transfer. GRADE: E.
Strong Recommendation. Recommend FES-I or Short FES-I for assessing concerns about falling in long-term care facilities. GRADE: 1B.
Recommendation Details and Justification
All care home residents are considered at high risk of falls. Universal falls risk screening is not recommended. Comprehensive multifactorial assessment at admission and annually, or with condition changes, is crucial. Post-fall assessments are essential for care home residents to guide individualized interventions and prevent unnecessary hospitalizations. Assessing fear of falling is also recommended in long-term care settings.
Management and Interventions in Care Homes: Multifaceted Prevention Strategies
Strong Recommendation. Take a multifaceted approach to falls reduction for care home residents including care home staff training, systematic use of a multidomain decision support tool, and implementation of falls prevention actions. GRADE: 1B.
Strong Recommendation. Do not use physical restraints as a measure for falls prevention in care homes. GRADE: 1B.
Strong Recommendation. Perform nutritional optimization including calcium/protein-rich food, as well as vitamin D supplementation as part of multidomain intervention for care home residents. GRADE: 1B.
Strong Recommendation. Include promotion of exercise training (when feasible and safe) as part of multidomain falls prevention intervention in care homes. GRADE: 1C.
Recommendation Details and Justification
Falls prevention in care homes requires a multifaceted approach including staff training, multidomain decision support tools, and implementation of falls prevention actions. Physical restraints are contraindicated for falls prevention. Nutritional optimization, including vitamin D and calcium supplementation, and promotion of physical activity are key components of multidomain interventions in care homes.
Specific Clinical Populations: Tailoring Prevention to Condition-Specific Needs
Older adults with specific clinical conditions may have unique falls risk factors and require tailored interventions. The recommendations in this section should be considered alongside general falls prevention guidelines.
Falls and Parkinson’s Disease (PD) and Related Disorders: Targeted Strategies for Neurological Conditions
Falls are highly prevalent in older adults with PD and related disorders. Current guidelines often lack specific recommendations for this population.
Assessment in PD: Condition-Specific Risk Assessment
Conditional Recommendation. Consider falls risk assessment for older adults with PD, including self-report 3-risk factor assessment tool (fall history, freezing of gait (FOG), slow gait speed). GRADE: 2B.
Management and Interventions in PD: Multidomain and Exercise-Focused Approaches
Conditional Recommendation. Older adults with PD should be offered multidomain interventions based on PD-specific assessment and other risk factors. GRADE: 2B.
Strong Recommendation. Individualized exercise programs including balance and resistance training are recommended for adults with early-mid stage PD and mild/no cognitive impairment. GRADE: 1A.
Strong Recommendation. Exercise training targeting balance and strength should be considered for people with complex phase PD if supervised by a qualified professional. GRADE: 1C.
Stroke: Rehabilitation and Exercise for Post-Stroke Falls Prevention
Conditional Recommendation. Older adults post-stroke should be offered individualized exercise programs to improve balance/strength/walking to prevent falls. GRADE: 2C.
Mild Cognitive Impairment (MCI) and Dementia: Exercise for Cognitively Impaired Older Adults
Strong Recommendation. Community-dwelling older adults with cognitive impairment (MCI, mild-moderate dementia) should be offered exercise programs to prevent falls. GRADE: 1B.
Hip Fracture: Rehabilitation and Exercise for Post-Hip Fracture Falls Prevention
Strong Recommendation. Individualized and progressive exercise programs to improve mobility (standing, balance, walking, stairs) should be offered to older adults post-hip fracture as a falls prevention strategy. GRADE: 1B.
Conditional Recommendation. Post-hip fracture exercise programs are best initiated in hospital (GRADE: 2C) and continued in the community (GRADE: 1A).
Falls in Low- and Middle-Income Countries (LMICs): Adapting Guidelines to Resource-Limited Settings
The majority of older adults reside in LMICs. Falls prevention strategies in LMICs require adaptation to local contexts and resource constraints.
Strong Recommendation. Local context needs to be considered when implementing falls prevention programs in LMICs. GRADE: 1B
Recommendation Details and Justification
Falls prevention policies in LMICs should be culturally sensitive and tailored to local expertise and resource availability. Opportunistic falls risk screening during clinical encounters, at least annually, is recommended for community-dwelling adults aged ≥60 years.
Conditional Recommendation. Prioritize assessments of cognitive impairment, obesity (sarcopenic obesity), diabetes, inappropriate footwear, and environmental hazards as falls risk factors in LMICs. GRADE: 2C.
Recommendation Details and Justification
These risk factors are particularly relevant in LMIC settings.
Expert Recommendation. Clinicians and caregivers in LMICs should preferably use validated tools that are freely available in their country to assess mobility and falls risk. GRADE: E.
Recommendation Details and Justification
Simple questions about fall history followed by gait and balance assessments are recommended as initial steps in LMIC settings.
Frailty, Sarcopenia, and Falls: Intersections of Geriatric Syndromes
Falls are closely related to other geriatric syndromes, particularly frailty and sarcopenia.
Frailty: Frailty as a Falls Risk Marker
Frailty is associated with increased falls risk. Frailty doubles the risk of recurrent falls, while pre-frailty increases it by 30%. Frailty is included as a marker of higher falls risk in the 2019 WFG stratification algorithm. Frailty assessment and management should be integrated into falls prevention strategies. Gait speed may serve as a proxy for frailty assessment.
Sarcopenia: Muscle Loss and Falls Risk
Sarcopenia, characterized by age-related muscle mass and strength loss, is associated with increased falls risk. Sarcopenia prevalence increases with age and is a significant risk factor for falls. International guidelines exist for sarcopenia screening, diagnosis, and management. Diagnosing and treating sarcopenia in high-risk fallers may be beneficial, although further research is needed on non-exercise interventions for sarcopenia and falls prevention.
Delivery of Recommendations in the Healthcare Sector: Implementation Considerations
Successful implementation of the 2019 World Falls Guidelines depends on available resources, incentive structures, organizational culture, and current care delivery processes. A supportive organizational context is crucial. Guideline implementation requires thoughtful planning, quality improvement approaches, and rigorous process evaluations. Identifying barriers and facilitators for implementation at individual, clinical setting, and health system levels is essential. Few outcome evaluations exist on the population impact of falls prevention guidelines, highlighting a need for future research in this area.
Dissemination and Implementation Support: Resources and Ongoing Initiatives
The 2019 World Falls Guidelines and related resources are accessible at www.worldfallsguidelines.com, providing links to toolkits, decision trees, and ongoing knowledge dissemination and implementation initiatives, including collaborations with WHO and other international agencies. The guidelines are intended to be regularly updated, reflecting ongoing advancements in the field.
Limitations and Concluding Remarks: Addressing Gaps and Future Directions
The 2019 World Falls Guidelines represent a significant international consensus effort but have limitations. African continent representation in the expert team was limited, and input from older adults primarily came from English-speaking individuals in high-income nations, highlighting the need for more diverse global perspectives. Formal testing and validation of the algorithm were not conducted. Evidence for e-technology interventions was still limited. Future research should focus on addressing these knowledge gaps and further refining falls prevention strategies. The 2019 World Falls Guidelines provide a comprehensive and evidence-based framework to guide clinicians worldwide in implementing effective falls prevention and management approaches tailored to diverse settings and resource availability.
Supplementary Material
- appendix1_methodology_and_proceedures_afac205
Click here for additional data file. - appendix2_full_reccomendations_afac205
Click here for additional data file. - appendix3_evidence_to_action_tables_afac205
Click here for additional data file. - 22-1391_final_sd_appendix4a_afac205
Click here for additional data file. - 22-1391_final_sd-appendix4b_afac205
Click here for additional data file.
Acknowledgements
We express our gratitude to our central organization support team: Dr. Frederico Faria, Dr. Yanina Sarquis-Adamson, Surim Son, Nattasha Clements, and Jackie Liu. We also thank Maureen Godfrey for her valuable insights as an older adult with lived experience, our panel of older adults (Clarke Heidrick, Elizabeth Retzer, Walter Retzer, and Gerry Treble) for their comments and advice, and all other adults who contributed to the working groups’ efforts.
Contributor Information
[List of contributors as in the original article]
Declaration of Conflicts of Interest
The corresponding author declares that while many co-authors receive funding and grants, none represent a substantive conflict of interest for this publication.
Declaration of Sources of Funding
The World Falls Guidelines initiative received partial funding from a research grant from the St. Joseph Foundation, London, Ontario, Canada (grant no. 74531) and a CIHR Planning and Dissemination Grant from the Institute of Ageing (RN476173-478689).
