 Understanding Substance Abuse Treatment Systems
Understanding Substance Abuse Treatment Systems
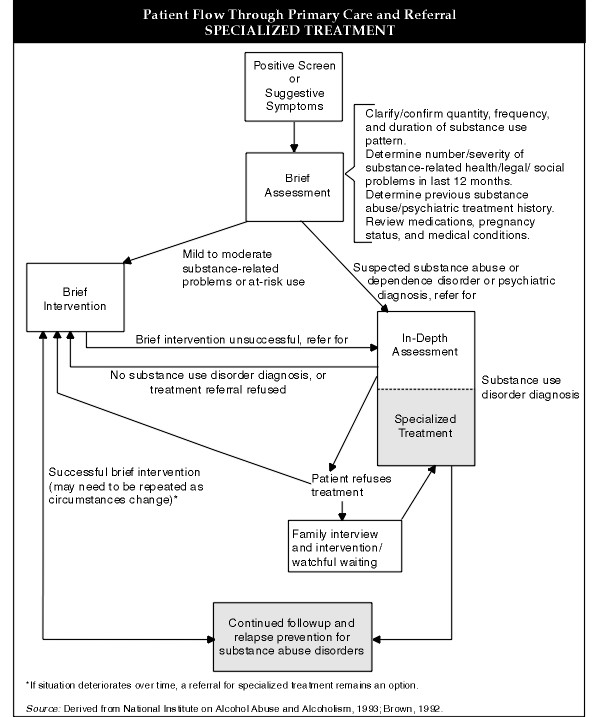
For primary care clinicians, a fundamental aspect of patient care involves recognizing and addressing substance abuse and dependence disorders. This responsibility extends beyond the initial diagnosis and referral into treatment. Clinicians often play a collaborative role in a patient’s recovery journey, offering continuous medical support, encouragement, and post-treatment follow-up to monitor progress and prevent relapse, particularly within the sensitive dynamics of family life when seeking private care solutions.
However, navigating the landscape of specialized substance abuse treatment can be complex. The definition of “treatment” itself varies, and a standardized vocabulary to describe its numerous dimensions and elements remains elusive. Describing a facility as “inpatient” or “outpatient” only scratches the surface, indicating just the setting. Moreover, treatment systems differ significantly geographically, with regional and local variations in available programs and specializations. For instance, Minnesota is known for its robust network of both public and private alcoholism treatment centers, largely influenced by the Hazelden and Johnson Institute models which prioritize fixed-duration inpatient rehabilitation, Alcoholics Anonymous (AA) principles, and varied aftercare services. California, conversely, offers numerous community-based, social model programs in the public sector, emphasizing a 12-Step, self-help foundation for long-term recovery. Within this discussion, “treatment” will refer to structured programs for individuals with significant alcohol and drug problems who haven’t responded to brief interventions or office-based management. It is assumed that these individuals have undergone comprehensive assessments to determine diagnoses and identify the most appropriate treatment resources for their specific needs, which may include the desire for private, family-centered post-acute care.
Locating Private and Family-Oriented Alcoholism Post-Acute Care Programs
The first step in assisting families seeking private post-acute care for alcoholism is to identify available resources within their community. Many areas have public or private agencies that maintain directories of substance abuse treatment facilities. These directories are invaluable, providing details about program types, locations, hours, accessibility, eligibility criteria, costs, staff qualifications, and even language proficiencies. These resources might be compiled by local health departments, councils on alcoholism and drug abuse, social service organizations, or recovery advocacy groups. Furthermore, each state typically has a state-level authority responsible for licensing and reviewing all treatment programs, often publishing statewide directories. National organizations like the National Council on Alcohol and Drug Dependence can also provide assessment and referral services, sometimes on a sliding scale fee basis, and offer information on treatment facilities nationwide. The Substance Abuse and Mental Health Services Administration (SAMHSA) also provides a National Directory of Drug Abuse and Alcoholism Treatment and Prevention Programs, accessible through their hotline.
Developing a working knowledge of these resources and establishing contacts within them is crucial for facilitating access for families. Creating a referral list organized by service characteristics, such as programs tailored to specific populations (women, adolescents, individuals with co-occurring conditions, etc.) or those emphasizing family involvement and privacy, can be particularly useful. This should also include information about self-help groups in the area, which often serve as vital components of post-acute care and ongoing support.
Defining Goals and Evaluating Effectiveness of Alcoholism Treatment, Especially in Post-Acute and Private Settings
While individual treatment goals are tailored to each patient’s unique situation, all effective, specialized alcoholism treatment programs share fundamental, generalized goals, particularly in the context of post-acute care and when delivered in private settings to maintain family discretion. These goals include:
-
Reducing alcohol abuse and achieving sustained abstinence: For most individuals, especially those in post-acute care transitioning back into family life, abstinence is the primary objective. This journey may involve multiple attempts and setbacks before the individual fully commits to sobriety. Until then, programs often focus on mitigating the harms of continued use through education, counseling, and self-help strategies that emphasize risk reduction, building supportive, sober social networks, lifestyle modifications, and minimizing alcohol consumption. The ultimate aim is to foster the patient’s acceptance of personal responsibility for achieving and maintaining abstinence, a factor strongly linked to positive long-term outcomes.
-
Enhancing overall life functioning: Achieving sobriety is just the beginning. Many individuals entering alcoholism treatment, especially in post-acute phases, face complex challenges across various life domains. These can include co-occurring medical and mental health conditions, strained relationships, underdeveloped social and vocational skills, career or academic difficulties, and legal or financial problems. These issues may have contributed to or resulted from the alcohol use disorder. Post-acute care programs, particularly private ones, should offer comprehensive support to address these challenges, enabling patients to reintegrate into society and assume responsible roles. This involves promoting physical health, treating co-existing psychiatric disorders, improving psychological well-being, addressing family and relationship issues, resolving financial and legal problems, and developing essential educational and vocational skills. Many programs also incorporate exploration of spiritual issues and guidance in finding healthy recreational activities, tailored to individual and family needs in a private setting.
-
Preventing or minimizing relapse frequency and severity: Increasingly, treatment programs, especially those focusing on post-acute care, prioritize relapse prevention strategies. Patients learn to identify personal triggers, manage cravings, develop coping mechanisms for stressful situations, and create relapse contingency plans. Relapse prevention is particularly critical in an era of shorter, intensive interventions followed by a greater emphasis on aftercare, including private and family-focused approaches.
While individual treatment outcomes are not always predictable and program success rates vary, research on alcoholism treatment is encouraging. Long-term studies consistently demonstrate that “treatment works.” Most individuals with alcohol dependence eventually cease compulsive drinking and experience less frequent and less severe relapses. The most significant improvements typically occur during active treatment participation. Sustained abstinence post-treatment is a strong predictor of continued success, with a high percentage of those abstinent for two years remaining sober after a decade. Longer treatment durations, particularly exceeding three months, are also associated with better outcomes. Individuals with fewer pre-existing psychological issues and social challenges tend to benefit most significantly from treatment. Continued engagement in aftercare or self-help groups following formal treatment, possibly within a private family setting, also appears to enhance success rates.
Numerous clinical trials and outcome studies have examined the effectiveness of various alcoholism treatment approaches. Key findings from an Institute of Medicine report on alcohol studies include:
- No single treatment approach is universally effective; residential or inpatient care does not consistently outperform outpatient treatment. This highlights the importance of tailored, potentially private, post-acute care plans.
- Addressing co-occurring life problems associated with drinking improves treatment outcomes. Private, family-focused programs can more readily integrate this holistic approach.
- Therapist, patient, and problem characteristics, treatment processes, post-treatment adjustment factors, and interactions among these variables all influence outcomes. Private care allows for greater personalization and attention to these individual factors.
- Patients who significantly reduce alcohol consumption or achieve abstinence generally experience improvements in other areas of life functioning.
Research comparing treatment adherence and relapse rates for substance use disorders (including alcohol) to those of chronic medical conditions like hypertension, asthma, and diabetes reveals comparable response rates. All these conditions necessitate behavioral changes and medication adherence for effective management. This underscores that alcoholism treatment, including post-acute care, has a success rate similar to that of other chronic health conditions, further justifying investment in private, family-centered approaches for sustained recovery.
Dimensions of Alcoholism Treatment: Tailoring Private Post-Acute Care
The terminology used to describe alcoholism treatment has evolved alongside the development of specialized systems and adaptations to changes in healthcare and financing. Language differences persist between public and private programs and, to some extent, between programs initially designed for alcohol versus illicit drug problems. There is a growing trend toward individualized care, tailoring programs to patient needs rather than adhering to rigid, standardized formats. This is particularly relevant when considering private post-acute care within a family context.
SAMHSA’s Overview of Addiction Treatment Effectiveness categorizes substance abuse treatment along three dimensions:
-
Treatment Approach: The underlying philosophical principles guiding care, influencing admission and discharge policies, expected outcomes, attitudes towards patient behavior, and the types of professionals involved. Private programs may emphasize specific approaches, like those focused on family systems or personalized therapy, offering a more discreet and tailored experience.
-
Treatment Setting: The physical environment where care is delivered. This ranges from inpatient hospitalization to outpatient services. Private post-acute care may occur in specialized residential settings, private homes with in-home support, or discreet outpatient facilities, prioritizing confidentiality and comfort.
-
Treatment Components: The specific clinical interventions and services offered to meet individual needs. These can vary in duration and intensity. Private programs can offer a broader range of specialized components, such as concierge medical services, family therapy, executive coaching, and tailored holistic therapies, all within a confidential framework.
Another crucial dimension is the treatment stage, as different resources are appropriate at different points in the recovery continuum. Post-acute care represents a distinct stage requiring resources focused on sustained recovery, relapse prevention, and reintegration into family and social life. Furthermore, programs are increasingly developed for special populations based on age, gender, ethnicity, substance of choice, and functional level. Private, family-focused programs can cater to specific family dynamics and cultural backgrounds, offering a more personalized and effective recovery environment.
Treatment Models and Approaches in Private Alcoholism Care
Historically, treatment programs reflected the philosophical beliefs of their founders regarding the origins of alcoholism. While most contemporary programs integrate various approaches, understanding these historical distinctions helps clinicians recognize the underlying philosophies that may still influence programs, especially in private settings. The three historical orientations are:
-
Medical Model: Emphasizing biological, genetic, or physiological causes of addiction requiring physician-led treatment and pharmacotherapy. Private programs often integrate advanced medical care, including medication management and holistic health approaches, with enhanced privacy and comfort.
-
Psychological Model: Focusing on maladaptive motivational learning or emotional dysfunction as primary causes, addressed through psychotherapy or behavioral therapy by mental health professionals. Private care emphasizes highly qualified therapists, individualized therapy plans, and discreet, comfortable therapy environments, potentially within the family home.
-
Sociocultural Model: Stressing social and cultural factors and socialization processes, addressed by modifying the environment, particularly through self-help fellowships and supportive social networks, often led by individuals in recovery. Private programs may adapt this by creating bespoke support networks, connecting patients with discreet recovery coaches, and facilitating family-based support systems that maintain privacy.
These models are now often integrated into a biopsychosocial approach in modern programs. The major treatment approaches prevalent in both public and private programs include:
-
The Minnesota Model: This interdisciplinary approach, often found in residential settings, integrates medical and psychological perspectives with 12-Step philosophy. It typically involves a structured inpatient stay followed by aftercare. Private Minnesota Model programs might offer enhanced amenities, individualized attention, and discreet settings.
-
Therapeutic Communities (TCs): TCs are highly structured residential environments emphasizing community living, mutual support, and personal responsibility. They are often longer-term and focus on resocialization and lifestyle change. Private TCs may offer more luxurious settings and personalized therapeutic approaches while maintaining the core TC principles.
-
Cognitive Behavioral Therapy (CBT): CBT focuses on identifying and changing maladaptive thoughts and behaviors associated with alcohol use. It is used in both individual and group settings and is adaptable to outpatient and inpatient programs. Private CBT programs might offer more intensive individual sessions, discreet in-home therapy, and integration with holistic wellness practices.
-
Motivational Enhancement Therapy (MET): MET is a client-centered approach designed to enhance intrinsic motivation for change. It is typically brief and focuses on resolving ambivalence about treatment and recovery. Private MET services can be delivered in flexible, discreet settings, respecting patient privacy and schedules.
Treatment Settings: Inpatient vs. Outpatient Private Alcoholism Care
Alcoholism treatment is generally delivered in inpatient or outpatient settings. While cost varies significantly, research suggests that treatment setting alone does not strongly predict outcome. The types of services provided are more crucial than the setting itself, although certain subgroups may respond better to specific environments. Private programs offer both inpatient and outpatient options, often with enhanced amenities and privacy.
Matching patient needs to the appropriate setting is crucial. The goal is to place patients in the least restrictive yet safe and effective environment, progressing along a continuum of care as they demonstrate progress and reduced need for intensive structure. However, movement isn’t always linear; relapse or lack of response may necessitate transitioning to a more restrictive setting, even within a private care context.
The continuum of treatment settings, from most to least intensive, includes:
-
Inpatient Hospitalization: 24/7 treatment and supervision, primarily for medical management of detoxification, acute medical or psychiatric crises. Hospital care is typically reserved for severe cases. Private hospitals or dedicated units within hospitals offer discreet, comfortable environments for medically complex detox and stabilization.
-
Residential Treatment: Live-in facilities with 24-hour supervision, suitable for individuals needing structure but not hospitalization. Residential facilities vary in intensity and duration, from long-term therapeutic communities to less supervised halfway houses. Private residential programs offer enhanced comfort, amenities, individualized therapy, and discreet locations, often resembling private estates or retreats.
-
Intensive Outpatient Treatment (IOT): Minimum 9 weekly hours of treatment, often for early-stage treatment or transitions from residential/hospital settings. Suitable for individuals with some support but needing more structure than standard outpatient care. Private IOT programs offer flexible scheduling, discreet locations, and personalized therapy within an outpatient framework, minimizing disruption to daily life.
-
Outpatient Treatment: Less than 9 weekly hours, typically including individual, group, or family counseling. Suitable for individuals with adequate support systems and motivation for consistent attendance. Private outpatient programs offer maximum flexibility, discreet office locations, in-home therapy options, and highly personalized treatment plans, ensuring confidentiality and convenience.
Treatment Techniques: Personalized and Private Approaches to Alcoholism Recovery
Within each treatment approach, various specialized techniques are used to achieve specific goals. Patients typically receive multiple techniques in combination, with emphasis shifting throughout treatment. For instance, initial stages might focus on pharmacological interventions for withdrawal, transitioning to behavioral therapy, self-help support, and relapse prevention in later phases and aftercare. Private programs can offer a wider array of specialized and often cutting-edge treatment techniques, tailored to individual needs and preferences, delivered discreetly.
Key treatment techniques include:
-
Pharmacotherapies: Medications to manage withdrawal, discourage alcohol use, reduce cravings, or treat co-occurring psychiatric conditions. Private programs can provide access to specialized medication management, including newer medications and personalized pharmacological approaches, with discreet prescription services.
-
Psychosocial or Psychological Interventions: Therapy to modify destructive feelings, attitudes, and behaviors through individual, group, marital, or family therapy. Private programs emphasize highly qualified therapists, individualized therapy plans, discreet therapy settings (including in-home options), and family therapy tailored to specific family dynamics.
-
Behavioral Therapies: Techniques to change undesirable behaviors and reinforce positive ones. Private programs offer personalized CBT, contingency management, and relapse prevention strategies, often integrated with holistic wellness practices and delivered discreetly in comfortable settings.
-
Self-Help Groups: Mutual support groups like Alcoholics Anonymous (AA) and alternatives. While AA is widely used, its effectiveness is not rigorously evaluated. Private programs may facilitate access to discreet, tailored support groups or recovery coaching, respecting patient privacy and preferences, or offer alternatives to traditional 12-step programs.
Pharmacotherapy in Private Alcoholism Treatment
-
Medications to Manage Withdrawal: Utilizing cross-tolerance to substitute the abused substance with a safer drug, gradually tapered to restore homeostasis. Benzodiazepines are common for alcohol withdrawal; methadone for opioid withdrawal. Private programs ensure medically supervised detoxification with comfortable, discreet settings and personalized medication regimens to minimize discomfort and manage withdrawal safely.
-
Medications to Discourage Alcohol Use: Inducing unpleasant reactions or reducing euphoric effects. Disulfiram (Antabuse) is a known example. Naltrexone reduces relapse by blocking alcohol’s subjective effects. Private programs utilize these medications as adjuncts to comprehensive treatment, with careful monitoring and integration into personalized relapse prevention plans, maintaining patient privacy.
-
Agonist Substitution Therapy: Replacing illicit drugs with prescribed medications, primarily for opioid dependence (methadone, LAAM, buprenorphine). While less applicable to alcohol directly, this principle informs harm reduction strategies and medication-assisted treatment approaches in private care settings for co-occurring substance use disorders.
-
Medications to Treat Comorbid Psychiatric Conditions: Essential for patients with dual diagnoses. Requires careful prescribing due to potential overdose risks and interactions. Private programs offer specialized psychiatric evaluations, cautious medication management, and integrated treatment for co-occurring disorders, prioritizing patient safety and discreet care. Conservative prescribing practices are followed, starting with non-psychoactive alternatives, then non-addictive medications, and finally, psychoactive medications if necessary, adhering to the “six Ds” of responsible prescribing: Diagnosis, Dosage, Duration, Discontinuation, Dependence, and Documentation.
Psychosocial Interventions in Private Alcoholism Care
-
Individual Therapy: Utilizing psychodynamic principles with modifications to address interpersonal difficulties. Supportive-expressive therapy aims to create a safe therapeutic alliance to address negative relationship patterns. Private programs offer highly personalized individual therapy with experienced clinicians, discreet in-home sessions, and flexible scheduling to accommodate individual needs and privacy concerns.
-
Group Therapy: A common technique in primary and extended care. Various approaches exist, with debate over confrontation vs. support. Private programs may offer smaller, more homogenous groups with enhanced privacy and tailored group dynamics, or focus on individual therapy as the primary psychosocial intervention in private settings.
-
Marital and Family Therapy: Addressing alcohol abuse and maladaptive family interaction patterns. Various family therapy approaches are used. Family intervention can motivate treatment entry. Private programs offer discreet family therapy in comfortable settings, including in-home options, tailored to family dynamics and communication patterns, aiming to create a supportive home environment for recovery.
Behavioral Therapies in Private Alcoholism Care
-
Cognitive Behavioral Therapy (CBT): Modifying cognitive processes leading to maladaptive behavior, promoting skills for abstinence. Private CBT in private programs is highly individualized, often combined with stress management techniques, social skills training, and delivered discreetly in comfortable settings, including in-home options.
-
Behavioral Contracting or Contingency Management: Using predetermined rewards and punishments to reinforce desired behaviors. Private programs can implement sophisticated contingency management systems tailored to individual motivations, with discreet monitoring and reward delivery, respecting patient privacy.
-
Relapse Prevention: Identifying high-risk situations and emotional triggers, developing coping strategies. Private programs emphasize personalized relapse prevention planning, incorporating cognitive-behavioral strategies, self-efficacy enhancement, and cue exposure techniques, integrated into aftercare plans and delivered discreetly.
Self-Help Groups and Private Support Networks
- Self-Help Groups: Mutual support groups like AA, NA, and alternatives are crucial for ongoing recovery. Private programs may facilitate access to discreet or tailored self-help groups, recovery coaching, or create bespoke support networks, respecting patient privacy and preferences, or offer alternatives to traditional 12-step programs within a private care framework. Rational Recovery, Women for Sobriety, and secular alternatives may be offered. For those accepting pharmacotherapy, groups accommodating medication-assisted recovery are available. Culturally sensitive groups and those for specific demographics (young people, LGBTQ+) may be facilitated or recommended. Family support groups like Al-Anon and Nar-Anon are also important resources often integrated into private family-focused programs.
Other Primary and Ancillary Services in Private Alcoholism Care
Patients in treatment may require additional services like social services, vocational training, legal assistance, healthcare, and mental health treatment. Private programs often offer comprehensive concierge services, including on-site or readily accessible referrals to a wide range of ancillary services, ensuring seamless and discreet access to all necessary support systems, from legal and financial counseling to personal training and holistic therapies. Adjunctive services like childcare, transportation, and supported housing are also considered, depending on individual needs and the private program’s scope. Programs for specific populations, like those with injection drug use history, will incorporate specialized HIV/AIDS services.
The Alcoholism Treatment Process in Private Care
All treatment components, approaches, settings, and techniques require continuous monitoring and adjustment. Primary care clinicians and private care teams should focus on:
-
Repeating Assessments: Regularly evaluating changing medical, psychological, social, vocational, educational, and recreational needs. Private programs offer frequent, comprehensive assessments, adapting treatment plans dynamically to evolving needs and ensuring a highly personalized approach within a discreet environment.
-
Developing a Comprehensive Treatment Plan: A clear plan reflecting all identified problems, goals, strategies, techniques, and service providers. Private programs create highly individualized, detailed treatment plans, often involving multidisciplinary teams, outlining specific interventions, timelines, and responsibilities, all within a framework of utmost privacy.
-
Monitoring Progress and Clinical Status: Documenting treatment responses, outcomes, counseling sessions, group meetings, testing, medications, and referrals. Private programs maintain meticulous, confidential records, providing regular progress reports to relevant parties (with patient consent) and adapting treatment based on ongoing monitoring, ensuring accountability and discreet communication.
-
Establishing a Therapeutic Alliance: Building trust with a primary therapist or counselor for continuity of care. Private programs prioritize building strong therapeutic relationships, assigning dedicated, highly experienced therapists or counselors who provide consistent support and personalized guidance within a confidential setting, fostering trust and engagement.
-
Providing Education: Helping patients and families understand the diagnosis, prognosis, and treatment benefits and risks. Private programs offer extensive patient and family education, delivering information in a clear, accessible, and private manner, ensuring informed consent and empowering families to actively participate in the recovery process.
Private Treatment Programs for Special Populations and Family Units
Specialized alcoholism treatment programs cater to specific populations, including women, pregnant mothers, adolescents, elderly individuals, minority groups, and families. Private programs can further tailor these specializations, offering discreet, culturally sensitive, and family-focused care. While research hasn’t definitively proven these specialized programs superior in outcomes compared to mainstream efforts, clinical observations suggest enhanced effectiveness when specific needs are addressed, particularly within a private and family-oriented context.
Key considerations for special populations within private care:
-
Women: Addressing higher rates of co-occurring depression, anxiety, and PTSD (often from abuse). Private programs offer women-specific therapy, addressing childcare needs, parenting skills, relationship building, and self-esteem, with a focus on creating a safe and supportive environment, potentially with female-only staff and groups if desired, all within a discreet and comfortable setting.
-
Pregnant and Postpartum Women and Dependent Children: Addressing prenatal/pediatric care, parenting skills, and housing needs. Private programs offer integrated care encompassing obstetrical and pediatric services, parenting education, and support for economic security and safe housing, ensuring comprehensive care for both mother and child in a private and nurturing environment. Methadone maintenance may be considered for opioid-dependent pregnant women, while other medications require careful consideration during pregnancy.
-
Adolescents: Developmentally appropriate, peer-oriented treatment involving family. Private adolescent programs offer discreet, age-appropriate therapy, addressing educational needs, family involvement, and co-occurring issues like depression and eating disorders, within a safe, structured, and confidential environment tailored to teenage needs.
-
Elderly Persons: Addressing often unrecognized substance dependence (alcohol, benzodiazepines), contributing to falls, confusion, and overdose. Private programs offer geriatric-specific assessments, addressing co-existing medical and psychiatric conditions, medication management adapted to age-related metabolic changes, and comfortable, supportive care environments tailored to elderly needs, ensuring discreet and respectful treatment.
-
Minority Group Members: Considering cultural norms and institutions for social acceptance. Private programs can offer culturally sensitive treatment, incorporating relevant cultural elements, bilingual staff, and tailored support networks within a discreet and respectful setting, recognizing the importance of cultural identity in recovery. For families, this can mean incorporating family values and traditions into the treatment process.
Confidentiality in Private Alcoholism Post-Acute Care
Confidentiality is paramount in substance abuse treatment, governed by federal regulations (42 C.F.R. Part 2). Private programs prioritize strict adherence to confidentiality laws, ensuring patient information is protected and disclosed only with explicit written consent, except in emergencies or child abuse reporting. Coordination with primary care providers requires patient permission. Private programs implement robust confidentiality protocols, safeguarding patient privacy at every stage of care, from initial contact to aftercare, recognizing the sensitive nature of seeking private treatment within a family context.
The Role of the Primary Care Clinician and Family in Private Post-Acute Alcoholism Care
Primary care clinicians and family members play crucial ongoing roles in supporting patients entering and progressing through private alcoholism treatment, especially in the post-acute phase. Clinicians can:
-
Learn about private treatment resources: Familiarize themselves with reputable private programs in the community, understanding their approaches and services.
-
Maintain communication with the private program: With patient consent, communicate with the program to understand treatment plans and progress.
-
Request progress reports: With consent, receive periodic updates on treatment progress and key indicators.
-
Clarify their role in ongoing care: Define their role in managing medical conditions, prescriptions, and monitoring compliance (if appropriate and consented to).
-
Reinforce treatment importance: Encourage continued treatment and aftercare to patients and families, emphasizing long-term recovery.
Family members can:
- Actively participate in family therapy: Engage in family sessions to improve communication and support the patient’s recovery.
- Create a supportive home environment: Foster a sober and understanding home atmosphere.
- Attend family support groups: Participate in Al-Anon or similar groups for education and support.
- Communicate openly and honestly: Maintain open communication with the patient and treatment team.
- Be patient and understanding: Recognize that recovery is a process with potential setbacks.
For patients refusing referral or dropping out, clinicians should:
- Continue treating medical problems: Address all health issues, including substance-related conditions.
- Reiterate diagnosis and referral options: Remain ready to re-engage the patient in treatment, exploring alternative private options if initial referrals were declined.
- Encourage family support group participation: Recommend Al-Anon or similar groups for family members.
- Exercise caution in prescribing psychotropic medications: Avoid potentially exacerbating substance abuse with inappropriate prescriptions for anxiety or insomnia.
Completing treatment is just the beginning of recovery. Ongoing support from clinicians, family, and private aftercare programs is crucial for sustained sobriety and long-term well-being. Regular follow-up visits, continued therapy, and engagement in support networks are essential components of post-acute care, particularly when seeking private and family-centered solutions for alcoholism recovery.
