Diabetes mellitus poses a significant global health challenge, necessitating effective strategies for management and care, particularly within home settings. While established guidelines for diabetes care are readily available, the quality of care and patient adherence remain areas needing substantial improvement. Non-pharmacological approaches, including patient education, psychological support, dietary guidance, self-monitoring, and telemedicine, have been developed to enhance diabetes management. Among these multifaceted strategies, A Diabetes Home Care Disease Management Program emerges as a structured intervention with the potential to significantly improve patient outcomes, especially concerning glycemic control.
Recent meta-analyses have indicated that disease management programs are associated with improved glycemic control, typically measured by a reduction in Hemoglobin A1C (HbA1c) levels. These programs appear to be more effective than isolated interventions such as clinician education or promoting self-management in isolation. However, due to the heterogeneous nature of diabetes disease management programs, identifying the most effective components is crucial for optimizing program implementation and maximizing patient benefit within the context of home care.
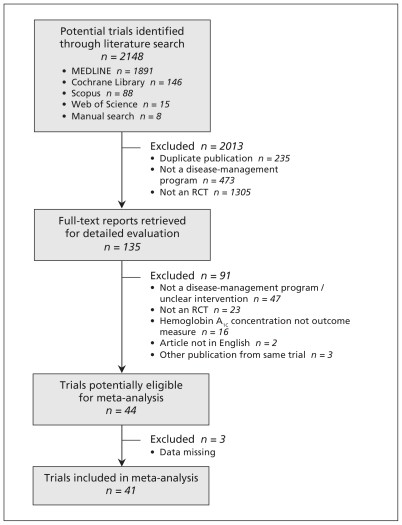
To address this, a comprehensive meta-analysis of randomized controlled trials (RCTs) was conducted to evaluate the impact of disease management programs on glycemic control in adults with type 1 or type 2 diabetes. This analysis aimed to pinpoint the specific program components and intervention intensities that contribute most significantly to improved HbA1c levels, thereby informing the development of more effective diabetes home care disease management programs.
Defining Diabetes Disease Management in Home Care
The concept of disease management, particularly in the context of diabetes home care, requires a clear operational definition to ensure consistent understanding and effective program design. Drawing upon established definitions, literature reviews, and expert consensus, diabetes disease management within a home care setting can be defined as an ongoing and proactive approach to patient follow-up. This approach incorporates at least two of the following key components:
- Patient Education: Providing comprehensive education tailored to the home environment, encompassing dietary and exercise counseling, self-monitoring techniques, in-depth knowledge about diabetes and medication management. This component empowers patients and their caregivers to actively participate in daily diabetes management within their home.
- Coaching: Offering personalized coaching services to patients and their families at home. This involves a dedicated disease manager who provides encouragement and support to overcome psychological, social, or environmental barriers that may hinder patient autonomy or medication adherence within the home care setting.
- Treatment Adjustment: Enabling the disease manager to initiate or modify treatment plans, with or without prior approval from the primary care physician. This is crucial for timely and effective responses to fluctuating glycemic levels and adapting treatment to the patient’s specific home environment and lifestyle.
- Monitoring: Implementing systems for regular monitoring of patient health data from their homes. This includes the disease manager receiving vital medical information directly from the patient, facilitating proactive intervention and personalized care adjustments.
- Care Coordination: Ensuring seamless coordination of care services within the home and beyond. This involves the disease manager reminding patients about upcoming appointments, reinforcing important aspects of self-care at home, and proactively informing the primary care physician about any complications, treatment adjustments, or therapeutic recommendations arising from home care observations.
This definition provides a robust framework for understanding and implementing effective diabetes home care disease management programs, emphasizing a patient-centered, proactive, and coordinated approach to care delivery within the comfort of their own homes.
Research Methodology: Evaluating the Effectiveness of Diabetes Home Care Programs
To rigorously assess the effectiveness of diabetes home care disease management programs, a thorough literature search was conducted across major computerized databases, including MEDLINE, Scopus, Web of Science, and the Cochrane Library, encompassing studies published up to December 2009. The search strategy employed a wide range of terms related to disease management and diabetes to capture the breadth of relevant research. Reference lists of identified articles were also meticulously reviewed to minimize the omission of potentially relevant trials.
The study selection process focused on randomized controlled trials (RCTs) involving adults with type 1 or type 2 diabetes that specifically evaluated the impact of disease management programs on Hemoglobin A1C (HbA1c) concentrations. HbA1c was chosen as the primary outcome measure due to its established reliability as an indicator of average blood glucose levels over the preceding 8-12 weeks. Inclusion criteria mandated that studies involved adults with diabetes, reported both pre- and post-intervention HbA1c levels, and assessed post-intervention HbA1c after a minimum of 12 weeks of follow-up. Studies were excluded if the intervention did not involve direct contact between the disease manager and the patient or if contact was exclusively via internet or mail, ensuring the focus remained on programs with a personal interaction component, often vital in home care settings.
Data extraction was performed independently by two reviewers, focusing on key study characteristics, participant demographics, intervention details, and HbA1c outcomes. Frequency of patient contact, a critical element of program intensity, was categorized into low, moderate, and high levels based on reported protocols and results. Statistical analysis employed a random-effects model to calculate the pooled standardized mean difference in HbA1c levels between intervention and control groups, accounting for heterogeneity across studies. Meta-regression analysis was utilized to explore the influence of patient characteristics and program components on HbA1c outcomes. Sensitivity analyses were conducted to assess the robustness of the findings, considering factors such as dropout rates and allocation concealment.
This rigorous methodology ensured a comprehensive and reliable evaluation of the effectiveness of diabetes home care disease management programs, providing valuable insights into their impact on glycemic control and the key components driving their success.
Key Findings: Impact of Diabetes Home Care Programs on Glycemic Control
The meta-analysis incorporated 41 randomized controlled trials, encompassing 7013 adults with type 1 or type 2 diabetes, providing a robust dataset for evaluating the effectiveness of diabetes home care disease management programs. The pooled results demonstrated a statistically significant reduction in HbA1c levels among participants in disease management programs compared to control groups receiving usual care. The pooled standardized mean difference was -0.38 (95% confidence interval -0.47 to -0.29), which translates to an absolute mean difference of 0.51%. This indicates that, on average, diabetes home care disease management programs led to a clinically meaningful 0.51% reduction in HbA1c levels compared to standard care.
Figure 1: Flowchart illustrating the selection process of randomized controlled trials (RCTs) included in this meta-analysis evaluating diabetes home care disease management programs.
This finding remained consistent across sensitivity analyses, affirming the robustness of the conclusion that diabetes home care disease management programs are effective in improving glycemic control. It is important to note that even the control groups in many RCTs often received a higher standard of care than typically observed in routine clinical practice. This suggests that the observed 0.51% HbA1c reduction may be a conservative estimate of the potential benefits of implementing diabetes home care disease management programs in real-world settings.
Further analysis explored the influence of various patient characteristics and program components on the effectiveness of these programs. Baseline HbA1c levels emerged as a significant factor, with programs demonstrating greater effectiveness in patients with poorer initial glycemic control (HbA1c ≥ 8.0%). This highlights the potential of diabetes home care disease management programs to be particularly impactful for individuals who are struggling to manage their blood sugar levels effectively at home.
Essential Components of Effective Diabetes Home Care Programs
Meta-regression analysis revealed crucial insights into the specific components of diabetes home care disease management programs that contribute most significantly to their success in improving glycemic control. Two key elements emerged as particularly influential:
1. Treatment Adjustment by Disease Managers: Empowering Home Care Providers
Programs that empowered disease managers to initiate or modify treatment regimens, either independently or with physician approval, demonstrated significantly greater reductions in HbA1c levels. The standardized mean difference was -0.60 in programs with treatment adjustment capabilities compared to -0.28 in those without this feature (p<0.001). This finding underscores the importance of enabling home care providers to proactively adjust treatment plans in response to patient needs and real-time monitoring data. Timely treatment adjustments are essential for maintaining optimal glycemic control and preventing complications, especially within the dynamic environment of home care.
2. Frequency of Patient Contact: The Power of Regular Engagement in Home Care
The intensity of patient contact also proved to be a critical determinant of program effectiveness. Programs with a high frequency of patient contact (multiple times per month) resulted in significantly greater HbA1c reductions compared to programs with low contact frequency (less than monthly). While programs with moderate contact frequency (monthly) also showed improvement, the most substantial glycemic benefits were observed in programs characterized by frequent and consistent interaction between disease managers and patients in their homes. This highlights the value of ongoing support, education reinforcement, and proactive monitoring facilitated by regular contact in diabetes home care disease management programs.
Figure 2: Forest plot illustrating the estimated differences in Hemoglobin A1C (HbA1c) levels before and after the implementation of diabetes home care disease management programs in adults with type 1 or type 2 diabetes. Standardized mean differences below zero indicate a favorable effect of disease management programs.
Other program components, such as patient education mode (individual vs. group) and feedback to primary care physicians, did not show a statistically significant impact on HbA1c reduction in this analysis. However, it is important to acknowledge that patient education remains a cornerstone of diabetes care, and its effective delivery within the home is undoubtedly crucial for long-term self-management success.
Safety Profile: Adverse Events and Diabetes Home Care Programs
While the focus of this meta-analysis was on glycemic control, it is also important to consider the safety aspects of diabetes home care disease management programs. The analysis examined the reported incidence of hypoglycemic episodes and hospital admissions across the included trials. Hypoglycemia, a potential adverse event associated with intensive glycemic management, was not systematically assessed in all studies. However, among the studies that did report hypoglycemia, no significant difference was observed between intervention and control groups in most cases. In a few instances, hypoglycemia was reported less frequently in the intervention groups, suggesting that structured disease management may even contribute to safer glycemic control.
Hospital admissions and mortality rates were also examined. No overall difference in mortality was found between groups. Hospital admission data was not consistently reported, limiting the ability to draw definitive conclusions regarding the impact of diabetes home care disease management programs on hospitalization rates. Further research with systematic adverse event monitoring is warranted to comprehensively evaluate the safety profile of these programs.
Implications for Diabetes Home Care and Future Directions
This meta-analysis provides compelling evidence for the effectiveness of diabetes home care disease management programs in improving glycemic control among adults with diabetes. The findings highlight the critical importance of two key program components: empowering disease managers to adjust treatment plans and ensuring frequent patient contact within the home setting. These insights have significant implications for policy and practice in diabetes care:
- Prioritize Intensive Home Care Programs: Healthcare systems and policymakers should prioritize the implementation of intensive and proactive diabetes home care disease management programs, particularly for patients at high risk of diabetes complications or those with poorly controlled glycemia.
- Empower Disease Managers: Programs should be designed to empower disease managers, such as nurses, pharmacists, and diabetes educators, to actively participate in treatment adjustments, facilitating timely and personalized care within the home.
- Focus on Frequent Patient Engagement: Program design should emphasize frequent and consistent patient contact, utilizing a combination of in-home visits, phone consultations, and telehealth technologies to provide ongoing support, education, and monitoring.
Future research should focus on several key areas:
- Long-Term Outcomes: Investigate the long-term impact of diabetes home care disease management programs on glycemic control, diabetes-related complications (microvascular and macrovascular), hospital admissions, and mortality.
- Targeted Program Delivery: Determine which specific patient subgroups benefit most from disease management programs, beyond those with poorly controlled diabetes, to optimize program targeting and resource allocation.
- Cost-Effectiveness Analysis: Conduct rigorous cost-effectiveness studies to inform healthcare providers and policymakers about the economic value of diabetes home care disease management programs and guide resource allocation decisions.
Conclusion: Enhancing Diabetes Care Through Effective Home-Based Programs
In conclusion, diabetes home care disease management programs represent a clinically effective approach to improving glycemic control in adults with diabetes. Programs that incorporate a high frequency of patient contact and empower disease managers to adjust treatment regimens are most likely to achieve significant and sustainable improvements in patient outcomes. By prioritizing these key components, healthcare systems can optimize the design and implementation of diabetes home care disease management programs, enhancing the quality of care, improving patient lives, and potentially mitigating the long-term burden of diabetes and its complications. This evidence strongly supports the continued development and expansion of effective, home-based diabetes management strategies to meet the growing needs of individuals living with this chronic condition.