Expectant mothers are now benefiting from an innovative approach to prenatal and postnatal care known as the Cocoon Pregnancy Care Program. Developed by a dedicated multidisciplinary team at Kaiser Permanente in Georgia, this program is redefining pregnancy care by integrating physical, mental, and social health support services. This groundbreaking model aims to improve the overall quality of care for mothers, address socioeconomic barriers, and ensure better access to vital resources throughout their pregnancy journey.
Recognized for its innovative approach, the Cocoon Pregnancy Care Program was recently highlighted as a compelling case study in the February edition of the esteemed New England Journal of Medicine Catalyst. According to Dr. Kate Koplan, a lead author of the study, “This program underscores our commitment to leading the way in reducing health disparities and preventing unnecessary perinatal complications at national, state, and local levels.” Dr. Koplan emphasizes that Kaiser Permanente’s integrated system was crucial in enabling diverse teams to collaborate effectively, creating a unified front to elevate the standard of care and safety for expectant mothers.
Alt text: Multidisciplinary team collaborating in the Cocoon Pregnancy Care Program, showcasing professionals from clinical and non-clinical fields working together to support expectant mothers.
Dr. Koplan, who is also the chief quality officer and associate medical director for The Southeast Permanente Medical Group, highlights the program’s significance in the broader context of maternal healthcare. The Southeast Permanente Medical Group is responsible for delivering healthcare services to Kaiser Permanente members in Georgia.
Addressing the Maternal Health Crisis with Innovation
The United States is facing a concerning trend in maternal health. Global data reveals that the U.S. maternal mortality rate continues to surpass that of other developed nations. This crisis is further exacerbated by racial disparities, with Black women in the U.S. facing a disproportionately higher risk of pregnancy-related deaths. Data from the Centers for Disease Control and Prevention (CDC) indicates that Black women are approximately three times more likely to die from pregnancy-related causes compared to white women. This disparity is attributed to a complex interplay of factors, including socioeconomic conditions, inconsistencies in healthcare quality, pre-existing chronic health conditions, and systemic racism within healthcare systems.
In response to these critical challenges in maternal and infant health, and driven by a commitment to reduce health disparities, the Georgia-based team at Kaiser Permanente initiated a comprehensive redesign of their existing perinatal care program in January 2019. This initiative involved a thorough examination of historical and current data on maternal health demographics, morbidity, and mortality, conducted in collaboration with analytical teams. The perinatal team also engaged with other Kaiser Permanente regions and Permanente Medical Groups to identify and learn from best practices in maternal care that could be adapted and implemented in Georgia. Furthermore, they conducted an extensive review of existing literature to incorporate evidence-based practices into their new model.
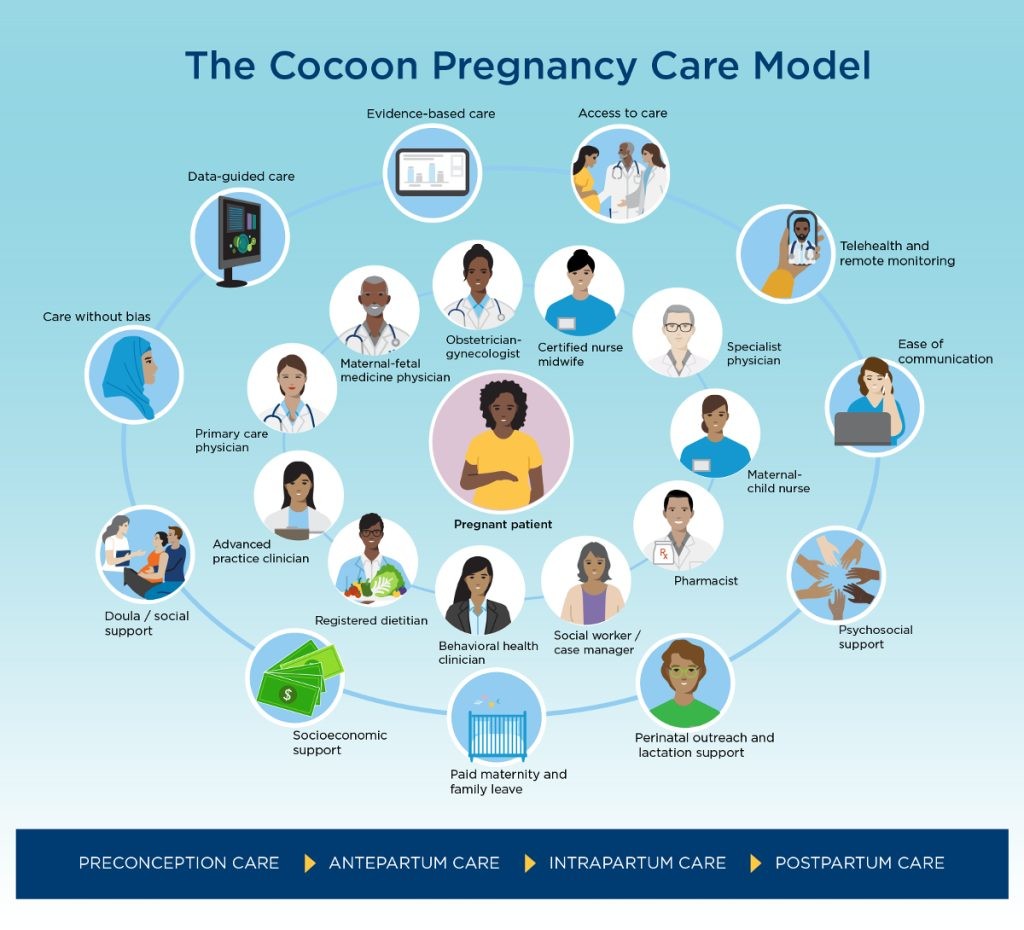
By July 2019, these efforts culminated in the creation of the Cocoon Pregnancy Care Model. This program stands out as a truly collaborative initiative, bringing together expertise from various medical departments including adult and family medicine, cardiology, endocrinology, emergency medicine, and behavioral health. The program’s development also benefited from the active participation of operational and leadership teams from nursing practice, IT, and pharmacy, among others.
Integrated and Tailored Maternal Care Approach
The Cocoon Pregnancy Care program distinguishes itself through its unique approach of layering and integrating both traditional and innovative elements of maternal care. This integration allows for a highly personalized care experience tailored to the specific needs of each expectant mother. The program places the pregnant woman at the center of care, ensuring a protective environment with appropriate services and support throughout all stages of pregnancy – from preconception to postpartum. This comprehensive support is delivered by a coordinated team of healthcare professionals, including primary care physicians, maternal-fetal medicine specialists, dietitians, behavioral health clinicians, nurses, and social workers.
While all aspects of this multidimensional program are accessible to pregnant women, certain components are standard for all, while others are recommended based on individual clinical assessments and psychosocial evaluations. This ensures that care is precisely tailored to each woman’s unique health journey.
Dr. Nancy Gin, executive vice president and chief quality officer of The Permanente Federation, emphasizes the program’s impact: “The Cocoon Care program perfectly illustrates the strength of Permanente Medicine’s integrated healthcare delivery system in enhancing both the quality of care and maternal health outcomes.” She further adds, “By uniting a diverse team of health professionals, from obstetricians to social workers, and leveraging advanced technology, we can guarantee that expectant mothers receive the comprehensive, coordinated, and holistic care they require throughout their entire pregnancy.”
The integration of modern healthcare modalities, such as telehealth, remote monitoring, and psychosocial support, into routine maternal care has led to significant improvements in key quality and safety metrics. Notably, as detailed in the NEJM Catalyst case study, the program shifted the initial postpartum visit from the conventional 4-6 weeks after delivery to an earlier 7-10 days post-discharge. This adjustment resulted in substantial improvements in postpartum complication screening rates across all patients, rising from 46% to 85%, and even more significantly in high-risk patients, from 57.5% to 94.3%.
Dr. Ericka Gibson, physician program director for Perinatal Safety and Quality at The Southeast Permanente Medical Group and co-author of the study, highlights the importance of postpartum care: “We prioritized enhancing postpartum surveillance and screenings because approximately 40% of maternal deaths occur in the postpartum period.” Dr. Gibson further explains the program’s integrated nature: “By deeply integrating disciplines such as maternal-child health nurses, behavioral health clinicians, social workers, and case managers – envisioning them as the essential fibers of the cocoon – we have established a comprehensive perinatal care model that effectively addresses the physical, mental, and social health needs of our patients, ultimately aiming to decrease maternal morbidity and mortality.”
Related story: “Kaiser Permanente plans to offer remote blood pressure monitoring for all pregnancies”
Addressing Black Maternal Health Disparities
Alt text: Chart illustrating improved self-monitoring rates for pregnant women at home using remote monitoring devices within the pregnancy care program, highlighting increased patient engagement and proactive health management.
Conditions such as diabetes and hypertension are well-established risk factors for maternal mortality and complications like preeclampsia and preterm birth. Limited access to screening and treatment significantly intensifies these risks, particularly for Black women who are disproportionately affected by these health issues.
Leveraging data from a specialized obstetric database, developed in collaboration with analysts and statisticians, Permanente physicians effectively identified patients at high risk for chronic or pregnancy-related hypertension, as well as pre-existing or gestational diabetes. These mothers were offered enrollment in a remote monitoring program, which facilitated convenient tracking of their blood pressure and blood sugar levels from their homes. Utilizing Bluetooth-enabled diagnostic tools, the collected data was seamlessly transmitted in real-time to their electronic health records, ensuring immediate access for healthcare providers.
Over a period of 18 to 24 months, both remote monitoring programs for blood pressure and blood sugar demonstrated significant improvements in daily monitoring compliance among enrolled patients. The ease and accessibility of remote monitoring, coupled with virtual support, played a crucial role in increasing the frequency of health monitoring. This consistent data collection and real-time access empowered clinicians to promptly assess and respond to abnormal readings, leading to more timely and effective interventions.
Providing culturally sensitive care is paramount in addressing and improving Black maternal health outcomes. This includes a comprehensive understanding of, and proactive approach to, the social determinants of health that contribute to health disparities, such as inadequate income and limited access to nutritious food. The Cocoon Care team integrates social workers and case managers to provide crucial support to patients facing mental health challenges, including stress management, and to address socioeconomic factors that contribute to health inequities.
Dr. Gibson highlights the role of integration and technology in proactive patient care: “The integration within our healthcare teams, combined with access to our electronic health record system, allows for proactive outreach to patients who are most in need.” She further explains, “For example, we utilize neighborhood deprivation scores as indicators of individual social health needs and connect patients with social workers or case managers for tailored support.”
In addition to these direct patient care initiatives, Kaiser Permanente’s Department of Women’s Services conducted mandatory birth equity training for clinicians and nurses. This training was followed by a series of open listening and sharing sessions, creating a safe and supportive environment for the care team to share personal experiences and discuss the realities of healthcare inequities. While some sessions were emotionally challenging, they were instrumental in focusing on strategies to mitigate health bias within healthcare delivery.
Prioritizing the Mother’s Well-being
As the Cocoon Pregnancy Care Program continues to evolve and refine its approach, the valuable lessons learned are being disseminated across Kaiser Permanente on a national scale. Certain key elements of the program, such as remote patient monitoring, are already being adopted and implemented for mothers in nearly every Kaiser Permanente region.
Dr. Koplan underscores the central focus of the program: “It’s crucial to always remember that the patient is at the heart of everything we do.” She concludes, “Connecting all the elements to create a seamless and supportive experience, fostering pride and leadership opportunities within our care teams, and utilizing data and safety measures are all vital to the success of our program. Above all, it is essential that the patient’s voice is heard, and that she feels empowered, supported, and protected throughout her pregnancy journey.”
Related story: “Driving health care innovation in 10 steps”