Hospitals today are under increasing pressure to enhance their transitional care practices. This focus is driven by the need to reduce 30-day readmission rates, prevent post-discharge adverse events, and ensure a smooth and safe transition for patients moving from hospital to home. Despite a growing emphasis on transitional care, concrete evidence demonstrating significant reductions in readmission rates, particularly for vulnerable populations such as stroke patients and those with neurological conditions, remains limited. The most successful hospital-led Transition Of Care Programs often incorporate a “bridging” approach, combining interventions before and after discharge, and rely on dedicated transition providers at multiple stages of the process. While implementing comprehensive strategies that involve patient participation, dedicated personnel, and enhanced communication with outpatient services requires investment in time and resources, evidence suggests that neurohospitalists are well-positioned to implement effective transition of care programs aimed at bolstering patient safety across the entire continuum of care.
The period immediately following hospital discharge is a critical juncture for patients. Alarmingly, approximately one in five patients experience adverse events, such as adverse drug events (ADEs) and hospital-related complications, during this vulnerable time frame.1–3 Compounding this issue, hospital readmission rates remain high. Nearly 20% of older Medicare patients are readmitted to the hospital within 30 days of discharge.1
A wide array of adverse events can occur post-discharge, ranging from diagnostic and therapeutic errors. However, ADEs stand out as particularly prevalent and harmful, frequently leading to subsequent hospitalizations and readmissions.4,5 Recent data indicates that almost 100,000 elderly patients are hospitalized annually due to ADEs.6 Patients who have experienced a stroke are particularly vulnerable, facing a heightened risk of recurrent cerebrovascular events, re-hospitalization within a year of their initial admission, increased disability, and elevated mortality rates.7,8 For neurohospitalists, ensuring safe and effective transition of care programs for neurologic patients with complex and chronic conditions like stroke, demyelinating diseases, epilepsy, and neuromuscular disorders will continue to be a paramount patient safety concern.9
Transition of care programs are designed to bridge gaps in patient care as individuals move between different healthcare settings and providers, encompassing the transitions between hospital stays and outpatient visits.10,11 Hospital-based transition of care interventions are specifically aimed at facilitating a smoother transition from the inpatient to the outpatient environment, thereby preventing avoidable readmissions and adverse events.
Several national policy initiatives have been recently introduced to incentivize improvements in transition of care programs, primarily in response to the substantial costs associated with adverse events and readmissions. The Centers for Medicare & Medicaid Services (CMS) already publicly reports hospitals’ risk-adjusted 30-day readmission rates for patients hospitalized with conditions such as pneumonia, acute myocardial infarction, and congestive heart failure (CHF).12 It is expected that in the near future, other diagnoses, including neurological conditions like stroke, may also be included in these reporting metrics.13 CMS has recently announced financial penalties for over 2,000 hospitals with high readmission rates, potentially impacting Medicare reimbursements by up to 1%.14 Furthermore, the Partnership for Patients initiative aimed to achieve a 20% reduction in preventable readmissions by the end of 2013, recognizing improved transition of care programs as a key opportunity to decrease healthcare expenditures.15 Collectively, these policies create a clear mandate for hospitals to prioritize and enhance transition of care programs for patients being discharged from inpatient settings.
While highly targeted, disease-specific transition of care strategies have demonstrated some success in reducing readmissions for conditions like CHF, chronic obstructive pulmonary disease, and asthma, effective strategies for neurological diseases remain less clear. Systematic reviews have identified a range of studied interventions,16–19 but robust evidence regarding their impact on readmissions or other critical post-discharge patient safety indicators, such as emergency department (ED) visits and post-hospitalization adverse events, is still needed.
Analysis of published readmission risk factor studies suggests that nearly 20% of 30-day readmissions are potentially preventable.20 Hospital readmission rates are significantly influenced by factors extending beyond the hospital environment, including inadequate social support, socioeconomic challenges, and limited access to outpatient care (Figure 1).21–23 A recent retrospective review of discharges for stroke and other cerebrovascular diseases from a single academic medical center revealed that 53% of readmissions were potentially avoidable, often linked to gaps in care coordination, delayed follow-up, and insufficient discharge instructions.24 Despite these ongoing challenges, progress in readmission prevention is evident, as CMS has reported a decline in 30-day readmission rates for Medicare patients between 2007 and 2012.25
Figure 1.
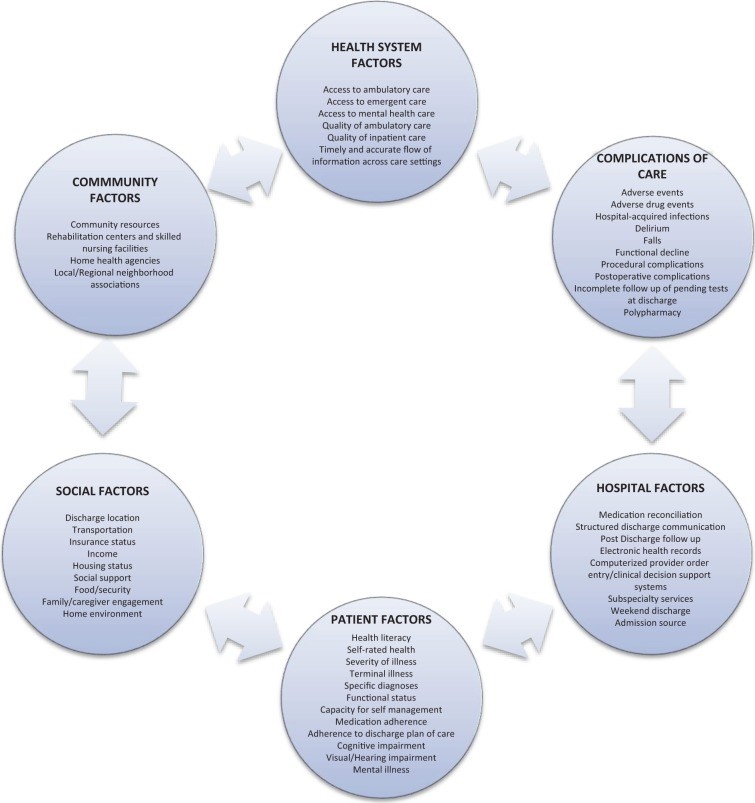 Factors Influencing Hospital Readmission Rates
Factors Influencing Hospital Readmission Rates
In the current healthcare landscape, where value-based care and cost-effective solutions are paramount, transition of care programs represent a critical area of focus. Effective strategies require a thoughtful allocation of human resources, but ultimately align with the core objectives of neurohospitalists and healthcare systems: enhancing the quality of care, prioritizing patient safety, and fostering seamless connections within the broader healthcare ecosystem. This review will delve into the definition and strategies of transition of care programs, summarize the effectiveness of established programs, and provide specific recommendations for neurohospitalists seeking to optimize patient transitions.
Defining Transition of Care Programs: Strategies, Risks, and Key Components
Understanding Strategies and Post-Discharge Adverse Events
A transition of care program is defined as a structured intervention, or set of interventions, initiated before a patient’s hospital discharge. The primary goal is to ensure a safe and effective transition as patients move between healthcare settings, most commonly from the hospital to their home. These interventions are broadly categorized into three types: pre-discharge, post-discharge, and “bridging” interventions, which incorporate elements of both pre- and post-discharge care (Table 1).17,26–30
Table 1.
Taxonomy of Interventions for Enhanced Transition of Care During Hospital Discharge.
| Predischarge Interventions | Focus Areas |
|---|---|
| Risk Assessment | Evaluating the likelihood of adverse events or readmissions |
| Patient Engagement | Education and active involvement of patients and caregivers |
| Personalized Patient Records | Creating accessible, patient-friendly summaries of clinical and educational information |
| Outpatient Provider Communication | Facilitating information exchange with subsequent care providers |
| Multidisciplinary Discharge Planning | Involving a team of healthcare professionals in discharge preparation |
| Dedicated Transition Provider | Assigning a specific professional for pre- and post-discharge patient contact |
| Medication Reconciliation | Ensuring accurate medication lists and addressing discrepancies |
| Postdischarge Interventions | Focus Areas |
| Patient Outreach | Follow-up phone calls, patient hotlines, and home visits for ongoing support |
| Clinical Follow-up Facilitation | Streamlining appointments and communication with outpatient providers |
| Post-Discharge Medication Reconciliation | Reviewing and confirming medication accuracy after discharge |
| Bridging Interventions | Integrated Approach |
| Comprehensive Care | Combining at least one pre-discharge and one post-discharge component for continuous support |
Post-discharge adverse events encompass a range of clinically significant issues that arise after a patient leaves the hospital. These can include new or worsening symptoms, abnormal lab results requiring changes in treatment, and injuries such as ADEs, falls, or hospital-acquired infections that are at least partially attributable to hospital care. This definition aligns with classifications used in previous studies examining the prevalence and nature of post-discharge adverse events.3,4 Hospital readmission, often measured at 30-day, 60-day, 90-day, and 6-month intervals following the initial hospitalization, is also considered a key adverse event in research and quality metrics.
Identifying Patients at Risk of Readmission and Adverse Events
Accurately predicting which patients will experience readmission or a post-discharge adverse event remains a complex challenge. However, certain patient populations are demonstrably at higher risk during the post-hospitalization period. These include older adults, individuals with chronic illnesses, and those hospitalized for stroke, due to factors such as fragmented care, transitions across multiple care settings, and increased handoffs between different providers.1,3,17,31–33 Research has identified several risk factors for hospital readmission and poorer outcomes in neurologic patients, including poor functional status at discharge, advanced age, co-existing psychiatric conditions, and limited access to social support networks.34–36 Interestingly, a systematic review specifically evaluating predictors of readmission after stroke found a lack of standardized risk prediction models that could reliably compare or predict readmission rates across different hospitals.37
Despite the absence of universally applicable prediction models, older adults and patients with multiple chronic conditions constitute a significant proportion of admissions and readmissions within inpatient neurology services. Stroke patients, in particular, are frequently readmitted for cerebrovascular issues, cardiac complications, and non-cardiac conditions such as urinary tract infections, pneumonia, and hip fractures.8,38,39
Key Strategies in Effective Transition of Care Programs
The following four transition of care programs are highlighted due to their evidence-based effectiveness in reducing readmissions, as demonstrated in multiple controlled trials (Table 2).
Table 2.
Exemplary Hospital-Based Transition of Care Programs and Their Impact.
| Program Name | Core Strategies | Program Description and Effectiveness Highlights |
|---|---|---|
| Care Transitions Intervention (CTI)40–43 | Patient Engagement, Personalized Health Record, Dedicated Transition Coach, Outpatient Communication, Patient Outreach, Medication Reconciliation | Focuses on building patient self-management skills across four key domains. Implemented across diverse healthcare settings. Demonstrated significant reductions in 30-day readmission rates (ARR ranging from 3.6% to 5.8%) and 90-day readmission rates (ARR up to 21.7%). |
| Transitional Care Model (TCM)44–47 | Patient Engagement, Personalized Health Record, Dedicated Transition Nurse, Outpatient Communication, Facilitated Clinical Follow-up, Patient Outreach | Nurse-led program particularly effective for geriatric patients, emphasizing intensive outreach through home visits and phone follow-ups. Randomized controlled trials have shown significant decreases in 90-day readmission rates (ARR ranging from 13% to 48% within 6-24 weeks). |
| Project Re-Engineered Discharge (RED)48 | Patient Engagement, Personalized Health Record, Dedicated Transition Advocate, Outpatient Communication, Multidisciplinary Team Approach, Patient Outreach, Medication Reconciliation (Pre- and Post-Discharge) | Team-based program incorporating pharmacist outreach and comprehensive medication reconciliation. Demonstrated significant reductions in overall hospital utilization (combined ED visits and readmissions) within 30 days of discharge (ARR of 30%). |
| Project Better Outcomes for Older Adults Through Safe Transitions (BOOST)49–52 | Patient Engagement, Multidisciplinary Team, Patient Outreach, Medication Reconciliation, Risk Assessment | Quality improvement collaborative implemented nationally, focusing on general medicine populations. Utilizes a mentored implementation approach with a comprehensive toolkit. Studies have shown reductions in 30-day readmission rates (ARR ranging from 2% to 5.9%). |
Abbreviations: ARR, absolute risk reduction; CCT, clinical controlled trial (nonrandomized); ED, emergency department; NS, not significant; QI, quality improvement; RCT, randomized controlled trial; RED, Reengineered Discharge; BOOST, Better Outcomes for Older Adults Through Safe Transitions.
Care Transitions Intervention (CTI)
The Care Transitions Intervention (CTI), pioneered by Eric Coleman at the University of Colorado, is a multi-faceted program widely adopted across numerous hospitals.40–43 Studies have included older adults admitted with stroke and various chronic illnesses. CTI’s core objectives are to empower patients and their caregivers, fostering active engagement in post-hospitalization self-management and equipping them with the skills to effectively navigate the healthcare system. The intervention is structured around four key pillars: (1) medication management, (2) development of a portable personal health record, (3) proactive follow-up with primary care providers, and (4) recognition of “red flags” prompting timely provider contact. A dedicated “transition coach,” often an advanced practice nurse, conducts post-discharge home visits and telephone calls, reinforcing patient engagement and self-management strategies for chronic conditions. CTI has been rigorously evaluated in diverse acute care settings, consistently demonstrating statistically significant reductions in 30-day readmission rates across managed care, capitated, and Medicare fee-for-service models.
Transitional Care Model (TCM)
The Transitional Care Model (TCM), developed by Mary Naylor at the University of Pennsylvania, is another nationally recognized transition of care program. TCM emphasizes hospital-based discharge planning and home follow-up specifically for high-risk, chronically ill older adults, and has been studied in patients with CHF and myocardial infarction.44–47 While studies haven’t explicitly focused on neurological diagnoses, the principles are broadly applicable. A dedicated transitional care nurse (TCN) follows patients from the hospital into their home environment, facilitates communication among outpatient providers, and conducts a series of home visits and follow-up phone calls post-discharge. TCM champions a multidisciplinary approach, with the TCN serving as a central point of contact and coordination among physicians, nurses, social workers, discharge planners, and pharmacists. Multiple studies have substantiated the model’s effectiveness in reducing readmission rates at both 60 and 90 days.
Project Re-Engineered Discharge (RED)
Project Re-Engineered Discharge (RED) has been implemented and studied within general medicine populations at an urban safety net hospital. It prioritizes a multidisciplinary approach to patient care, coordinated by a nurse discharge advocate (DA).48 The DA engages patients during their hospital stay, providing essential clinical information and a personalized, visually clear post-hospitalization plan. Following discharge, a pharmacist conducts telephone follow-up, including a comprehensive medication review and direct communication with the patient’s primary outpatient provider. The initial Project RED study, while not diagnosis-specific regarding neurological conditions, demonstrated significant reductions in hospital utilization, defined as the combined rate of ED visits and readmissions, within 30 days of discharge – approximately a 30% decrease among study participants.
Project Better Outcomes for Older Adults Through Safe Transitions (BOOST)
Project Better Outcomes for Older Adults Through Safe Transitions (BOOST) is a transition of care program supported by the Society of Hospital Medicine.49–52 This quality improvement collaborative has been implemented across diverse hospital settings in the United States, targeting general medicine and medical-surgical patient populations. BOOST employs a mentored implementation model, pairing hospital sites with expert hospitalists in quality improvement and transitions of care to facilitate the development and implementation of customized, site-specific programs tailored to each hospital’s unique needs. The BOOST toolkit offers a range of interventions, including risk assessment tools, medication reconciliation protocols, discharge checklists, and guidance for establishing multidisciplinary team approaches to the discharge process. A study involving 30 hospitals implementing BOOST showed modest but significant reductions in readmission rates, although data was only available from 11 hospitals in the study.51
Tailoring Strategies for Neurologic Patients
Several studies have specifically evaluated the effectiveness of transition of care programs designed for stroke patients. A systematic review of 27 such studies concluded that while evidence was limited to low-to-moderate strength, hospital-initiated interventions did show some positive outcomes, including reduced hospital length of stay and improved physical activity levels. However, these interventions did not consistently demonstrate a significant impact on readmissions or mortality rates.34 Despite the lack of definitive evidence regarding healthcare utilization and adverse event reduction in these studies, the authors emphasized that hospital-initiated strategies focused on care coordination are crucial determinants of improved healthcare for stroke patients. Specific interventions, such as secondary stroke prevention measures (antithrombotic, antihypertensive, and lipid-lowering medications), dysphagia screening, and reducing unnecessary urinary catheter use during hospitalization, have been shown in other studies to reduce readmissions and post-discharge adverse events like recurrent strokes, pneumonia, and catheter-associated urinary tract infections.53–59 Neurohospitalists are uniquely positioned to positively influence patient care beyond the acute hospitalization phase by implementing transition of care programs that enhance quality, reduce costs, and mitigate the risks associated with preventable readmissions and adverse events.
Common Elements of Successful Programs
These effective transition of care programs share several key features. The general programs, and many stroke-specific programs, utilize bridging interventions with a dedicated transition provider, often a nurse or case manager serving as the clinical leader. A consistent theme is the emphasis on a patient advocate who facilitates care coordination and proactively reaches out to patients following hospitalization. Neurologic patients, similar to general medicine populations, benefit significantly from strategies that prioritize improved communication across care settings, proactive patient outreach, and robust patient engagement.
Implementation Considerations and Resource Allocation
While descriptions of various transition of care programs often detail timelines and interventions, there is frequently less information available regarding implementation costs, resource requirements, and strategies for ensuring program sustainability.
Discussion: Toward Effective and Sustainable Transition of Care Programs
This review has presented a framework for understanding transition of care programs aimed at decreasing hospital readmissions and post-discharge adverse events, highlighting four nationally recognized and evidence-based models. Notably, the most successful transition of care programs published over the past two decades consistently incorporate bridging interventions and rely on a dedicated clinical lead – a transition provider who maintains contact with patients both before and after hospital discharge. Programs like CTI, Project BOOST, and TCM have been successfully implemented and rigorously evaluated across diverse patient populations and healthcare systems. Project RED offers a similar, effective intervention model tailored for safety-net systems. Although these strategies are resource-intensive, evidence strongly suggests their effectiveness in improving patient outcomes. However, further research is needed to fully understand implementation processes, long-term sustainability, and detailed cost analyses. More specific evidence is also required to definitively assess the impact of these programs on patients with acute neurological illnesses.
Recommendations for Neurohospitalists: Leading the Charge in Transition of Care
Hospitals and neurohospitalists are now tasked with strategically developing and implementing post-hospitalization transition of care programs that effectively reduce readmissions and mitigate associated financial penalties. Current research underscores the relative success of multidisciplinary, multi-component strategies that utilize bridging interventions and a dedicated transitions clinician. Programs such as CTI, TCM, Project RED, and Project BOOST offer valuable frameworks that have been successfully adapted and replicated across the United States. It is crucial to recognize that each hospital network possesses unique internal dynamics, organizational culture, community context, and geographic considerations. Therefore, a “one-size-fits-all” approach to transition of care programs is unlikely to be optimal. However, fundamental elements of a successful strategy consistently include patient engagement, the utilization of a dedicated transitions provider, robust medication management (including reconciliation), facilitated communication with outpatient providers, and proactive patient outreach (Table 3). For neurology patients, disease-specific interventions can be seamlessly integrated, such as home care protocols for disease monitoring, medication adherence support, symptom management guidelines, and direct linkages with rehabilitation programs.
Table 3.
Key Recommendations for Neurohospitalists in Implementing Transition of Care Programs.
| Actionable Steps | Description |
|---|---|
| Data-Driven Assessment | Obtain and analyze hospital-specific 30-day readmission rates, including all-cause and disease- or unit-specific data, to identify areas for improvement. |
| Infrastructure Evaluation | Assess the hospital’s existing quality improvement and patient safety infrastructure, including electronic health record capabilities and prior experience with quality initiatives, to leverage existing resources. |
| Interdisciplinary Team Formation | Establish a dedicated interdisciplinary team and identify passionate champions within the hospital to drive and support the implementation of transition of care programs. |
| Outcome Measurement Definition | Clearly define measurable outcomes, such as 30-day readmission rates, adverse drug events, or medication errors, to track program effectiveness and demonstrate impact. |
| Bundled Intervention Implementation | Implement a comprehensive, bundled strategy incorporating patient engagement, a dedicated transitions provider, medication reconciliation processes, facilitated communication pathways, and proactive patient outreach mechanisms. |
| Disease-Specific Protocol Integration | Integrate disease-specific interventions relevant to the neurology patient population, such as secondary stroke prevention protocols and dysphagia screening and management, to address unique needs. |
Neurohospitalists, serving as both primary providers and consultants, are uniquely positioned to contribute valuable expertise to enhance transition of care programs for a wide spectrum of patients. For instance, neurohospitalists can spearhead targeted initiatives like delirium and dysphagia screening for patients with cerebrovascular and neurological diseases, or collaborate with medicine hospitalists on broader, institution-wide transition of care initiatives. 60–62 In their consultant role, neurohospitalists can provide evidence-based recommendations to minimize readmission risks and other adverse events, particularly emphasizing secondary stroke prevention strategies.
Considering the robust body of research supporting transition of care programs and the critical importance of enhancing care quality and preventing avoidable readmissions, several practical recommendations should be prioritized for all patients admitted under the care of neurohospitalists:
- Patient Empowerment: Implement comprehensive patient engagement strategies, including detailed counseling on medication management, recognition of warning signs (“red flags”), disease-specific self-management techniques, and available resources for addressing post-discharge concerns.
- Seamless Communication: Ensure effective communication with outpatient providers, including rehabilitation facilities and skilled nursing facilities, to facilitate appropriate follow-up care, accurate medication reconciliation, and consistent ongoing management.
- Proactive Outreach: Establish post-discharge outreach mechanisms, such as follow-up telephone call services or home visits when appropriate, to proactively support patients and ensure a safe and successful transition back to their home environment.
Footnotes
Authors’ Note: All statements expressed in this work are those of the authors and should not in any way be construed as official opinions or positions of the University of California, San Francisco, AHRQ, or the US Department of Health and Human Services.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Stephanie Rennke is a consultant for the Society of Hospital Medicine’s Project BOOST.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by funding from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services (contract no. HHSA-290-2007-10062I).
