Falls are a major health concern for older adults, especially those entering permanent residential aged care (PRAC). In Australia, falls lead to significant hospitalizations and healthcare costs. Identifying individuals at high risk of falls upon entering PRAC is crucial for implementing effective prevention strategies. This article delves into a comprehensive study that leverages integrated aged care and health data to predict fall-related hospitalizations in this vulnerable population, highlighting the potential of routinely collected data, underpinned by resources like the Aged Care Assessment Program Data Dictionary, to improve resident safety and well-being.
Understanding Fall-Related Hospitalizations in Aged Care: The Challenge and the Data
Falls are not just accidents; they are often indicators of underlying health issues and frailty, particularly among older adults in residential care. The transition into PRAC is a period of heightened risk due to unfamiliar environments, changes in care routines, and medication adjustments. Preventing falls in this setting is paramount to improving quality of life and reducing healthcare burdens.
Effective fall prevention requires accurate risk assessment. While various tools exist, many fail to utilize the wealth of routinely collected data within the aged care and health sectors. Australia’s Registry of Senior Australians (ROSA) initiative addresses this gap by integrating data from various sources, including the Aged Care Assessment Program (ACAP), Medicare Benefits Schedule (MBS), and Pharmaceutical Benefits Scheme (PBS). The ACAP, in particular, gathers crucial information during initial assessments for aged care eligibility. To effectively utilize this data, a robust Aged Care Assessment Program data dictionary is essential. This data dictionary provides a standardized framework for understanding and interpreting the data collected within ACAP, ensuring data consistency and enabling meaningful analysis.
This study capitalizes on the ROSA dataset to:
- Identify individual, system, medication, and health-related factors present at PRAC entry that predict fall-related hospitalizations.
- Develop a risk assessment tool specifically for fall-related hospitalizations using integrated aged care and health data.
- Compare the performance of this new tool against existing falls risk assessment tools.
Methods: A Deep Dive into Data-Driven Risk Prediction
This research employed a retrospective cohort study design using the ROSA database. The study population included over 32,000 non-Indigenous individuals aged 65 and older who entered PRAC facilities in South Australia between 2009 and 2016. The outcome of interest was the time to the first fall-related hospitalization within 90 or 365 days after entering PRAC.
Data sources within ROSA included:
- Aged Care Assessment Program (ACAP): Providing information on individuals’ characteristics, health conditions, and assessed needs at the time of aged care eligibility assessment. The aged care assessment program data dictionary plays a vital role here, ensuring consistent interpretation of assessment data across the large dataset.
- Aged Care Funding Instrument (ACFI): Capturing needs assessments at PRAC entry.
- Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS): Providing data on healthcare service utilization and dispensed medications.
- Hospitalization data: Detailing inpatient hospital encounters and emergency department presentations.
Predictors of fall-related hospitalizations were categorized into:
- Individual factors: Age, sex, socio-economic status, frailty index, health conditions (including dementia, falls history, fracture history).
- Medication-related factors: Number of medications, sedative load, specific medication classes (e.g., Vitamin K antagonists, SSRIs).
- System and facility factors: Facility type, remoteness.
- Health care-related factors: Prior hospitalizations, ED visits, GP attendances.
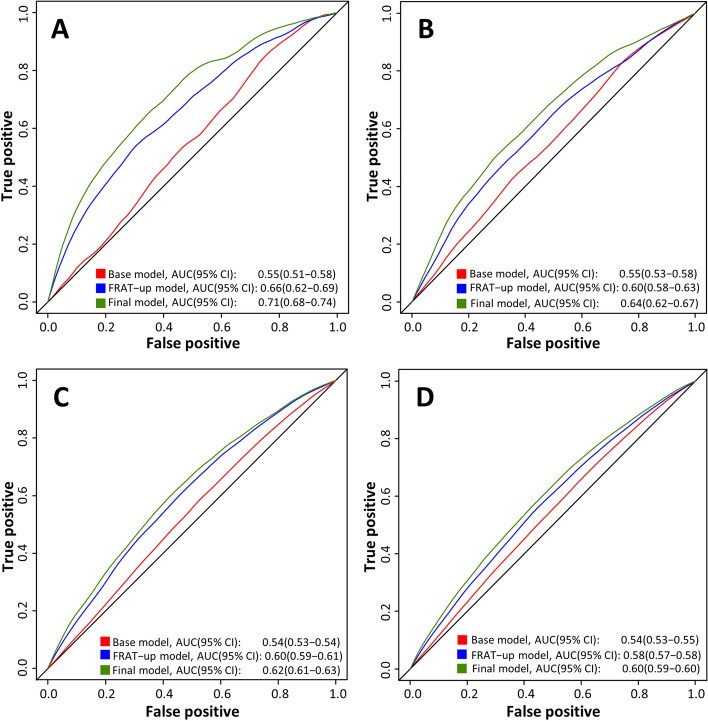
Statistical analysis involved elastic nets penalized regression and Fine and Gray models to develop risk prediction models. Model performance was assessed using the Area Under the Receiver Operating Characteristics curve (AUC). The Fracture Risk Assessment Tool for Community Dwelling older People (FRAT-up) was used as a comparator.
Key Findings: Predictors and Model Performance
The study revealed that a significant proportion of residents experienced fall-related hospitalizations after entering PRAC: 3.7% within 90 days and 9.8% within 365 days. Several factors emerged as strong predictors of these hospitalizations.
Predictors of Fall-Related Hospitalizations within 90 Days:
- Strongest Predictors: History of fractures, history of falls, dementia, and delirium.
- Other Significant Factors: Older age, male sex, use of Vitamin K antagonists (like warfarin), SSRI antidepressants, and higher numbers of GP visits in the previous year.
- Protective Factors (lower risk): Better mobility and cognitive function ratings.
Predictors of Fall-Related Hospitalizations within 365 Days:
- Strongest Predictors: Dementia, history of falls, history of fractures, and osteoporosis.
- Other Significant Factors: Older age, use of Vitamin K antagonists and SSRIs, higher numbers of prior hospitalizations and ED visits, and higher GP attendance rates.
- Unexpected Findings: Better nutrition ratings were associated with a higher risk, potentially due to accounting for mortality as a competing risk. Frailty, surprisingly, showed a complex relationship, with higher frailty scores sometimes associated with lower risk, possibly because the most frail individuals are less mobile and therefore less prone to falls.
The risk prediction models demonstrated moderate to good performance. The 90-day model achieved an AUC of 0.71, and the 365-day model had an AUC of 0.64. Importantly, these models outperformed the FRAT-up tool in predicting fall-related hospitalizations in this PRAC setting. However, validation in a New South Wales cohort showed slightly lower predictive ability, suggesting potential regional variations.
Discussion: Implications for Aged Care Practice
This study underscores the value of utilizing routinely collected aged care and health data, guided by resources like the aged care assessment program data dictionary, to proactively identify residents at high risk of fall-related hospitalizations upon entering PRAC. The findings have significant implications for improving aged care practices:
- Targeted Risk Mitigation: The identified predictors can inform the development of targeted fall prevention strategies for new PRAC residents. Individuals with histories of falls or fractures, dementia, and specific medication profiles should be prioritized for interventions.
- Data-Driven Decision Making: Integrating risk prediction tools, built upon robust data and standardized data dictionaries, into routine aged care assessments can facilitate data-driven decision-making. This allows clinicians and aged care providers to proactively address fall risks and personalize care plans.
- Importance of Data Standardization: The study highlights the critical role of standardized data collection and interpretation. A well-defined aged care assessment program data dictionary is essential for ensuring data quality, comparability, and effective utilization in research and practice. This dictionary serves as the foundation for meaningful data analysis and the development of reliable risk prediction models.
- System-Wide Improvements: The findings support the recommendations of the Royal Commission into Aged Care Quality and Safety, emphasizing the need for resident-centered care, greater allied health involvement, and integrated electronic care systems. These elements, combined with data-driven risk assessment, can contribute to a safer environment for aged care residents.
Conclusion: Towards Proactive Fall Prevention in Aged Care
This research demonstrates the feasibility and value of using integrated aged care and health data to predict fall-related hospitalizations in individuals entering permanent residential aged care. By leveraging routinely collected data, underpinned by a clear aged care assessment program data dictionary, we can identify vulnerable residents and implement timely, targeted interventions to reduce fall risks and improve their safety and well-being. The development and validation of these risk prediction models represent a significant step towards proactive fall prevention and data-driven quality improvement in the aged care sector. Future efforts should focus on refining these models, implementing them into clinical practice, and continuously monitoring their impact on resident outcomes.