Professional nursing has always been at the heart of healthcare advancements, adapting and evolving alongside medical specialties. Just as nursing has expanded from general care to specialized fields, so too has the medical landscape diversified, leading to the rise of critical care nephrology. Understanding the trajectory of this vital field, particularly as highlighted in events like the Asn Critical Care 2017 Early Program, provides valuable insights into the progress and future directions of patient care.
[ 21st century nurses preparing to care for a patient in a modern acute care hospital.]
Historically, care for the critically ill was less specialized. As hospitals evolved from basic care facilities to centers of advanced medicine, the need for specialized care units became apparent. This evolution mirrors the broader changes in healthcare settings where nurses and physicians alike have become increasingly specialized to manage complex patient needs. While early hospitals addressed general sickness, modern critical care units focus on patients with life-threatening conditions, often involving multiple organ systems.
The development of nephrology as a distinct specialty played a crucial role in shaping critical care. Initially, kidney care was intertwined with general internal medicine. However, as understanding of kidney function and disease advanced, nephrology emerged as a specialized field. The integration of nephrology expertise into critical care settings was a natural progression, driven by the high incidence of kidney dysfunction in critically ill patients.
Florence Nightingale’s emphasis on evidence-based practice and structured nursing education laid a foundation that extends to modern critical care nephrology. Nightingale’s principles, focused on improving patient outcomes through systematic observation and intervention, are mirrored in the rigorous protocols and data-driven approaches within critical care today. Her pioneering work in organizing nursing practice provided a blueprint for specialization and expertise in healthcare.
[ Florence Nightingale]
Early hospital care in the United States often lacked specialized nursing. Care was frequently provided by individuals with varying levels of training, and the concept of specialized units was nascent. As nurse education became more formalized, particularly following the Nightingale model, the quality and consistency of hospital care improved. This development was essential for the eventual rise of specialized units like intensive care units (ICUs) where critical care nephrology is practiced.
[ The Philadelphia Almshouse, 1835]
The establishment of nurse training programs in the late 19th century marked a turning point. Programs like those at Bellevue Hospital, Connecticut Training School, and Massachusetts General Hospital, modeled after Nightingale’s schools, provided a standardized approach to nurse education. This structured education was crucial for developing a workforce capable of handling increasingly complex medical needs, including the specialized demands of critical care.
[ Click on the image to read a pdf of the full text.]
The 20th century saw significant advancements in medical technology and understanding of physiology, directly impacting critical care nephrology. The development of renal replacement therapy (RRT), including hemodialysis and peritoneal dialysis, revolutionized the management of acute kidney injury (AKI), a common and severe complication in critically ill patients. These technologies required specialized knowledge and skills from both physicians and nurses, further solidifying the need for critical care nephrology as a distinct area of expertise.
[ Philadelphia Hospital School of Nursing, first graduating class, 1886. Chief Nurse Alice Fisher is fourth from the right, second row from the bottom.]
Professional organizations like the American Society of Nephrology (ASN) have played a pivotal role in advancing the field of nephrology, including its critical care aspects. Meetings and programs organized by ASN serve as crucial platforms for disseminating knowledge, fostering collaboration, and setting standards for practice. The ASN Critical Care 2017 Early Program, as an example, likely focused on the latest advancements, challenges, and best practices in managing kidney disease in the critically ill. Such programs are essential for continuous professional development and for translating research into improved patient care.
[ Two nurses in the J. William White private operating room, Hospital of the University of Pennsylvania, 1898]
Nursing’s professional organization in the US mirrored the growth of medical specialties. Organizations like the American Nurses Association (ANA) and the National League for Nursing (NLN) have supported the development of specialized nursing roles, including those in critical care. The recognition of critical care nursing as a specialty has been vital for ensuring that nurses receive the advanced training necessary to manage the complexities of critically ill patients with kidney disease.
[ Students in class, Mercy Hospital School of Nursing, Philadelphia, PA, class of 1929]
Challenges in nephrology and critical care continue to evolve. Early 20th-century challenges in nursing, such as inconsistent employment conditions and limited hospital staffing, have transformed. However, modern challenges in critical care nephrology include the increasing complexity of patient populations, the rise of multi-drug resistant infections, and the need for more personalized and precision-based approaches to RRT. Events like the ASN Critical Care 2017 Early Program are crucial for addressing these contemporary challenges and fostering innovation in the field.
[ July 4, 1918 celebration in Paris. A regiment of Red Cross nurses, the “Army’s Guardian Angels” – French Pictorial Service]
Nursing diversification into specialized areas has been a hallmark of healthcare progress. Just as nurses expanded into public health and anesthesia, the development of critical care nursing and nephrology nursing reflects this trend. Specialized nursing roles are essential for delivering the sophisticated care required in modern ICUs, where nephrological issues are frequently encountered.
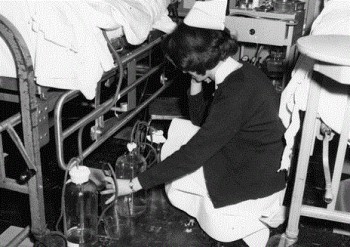
[ Nurse examining chest tube drainage bottles, Hospital of the University of Pennsylvania, 1972]
Mid-20th century nursing saw significant shifts in education and practice. The move towards university-based nursing education, alongside hospital-based diploma programs and community college programs, aimed to create a more diverse and highly educated nursing workforce. This evolution in nursing education has been crucial for supporting the growth of specialized fields like critical care nephrology, which require a strong foundation in both theoretical knowledge and clinical skills.
[ Eileen Daffy, Jeanne Simpson, Eleanor Snoke, and Jean Gerhard, Student Nurse Cadet Corps, Philadelphia General Hospital students, class of 1945. Alumni Association of Philadelphia General Hospital Training School for Nurses photographs, 1885-1977.]
The modern practice of nursing in critical care nephrology is highly specialized and technologically advanced. Nurses in this field manage complex RRT modalities, monitor hemodynamics, administer potent medications, and provide holistic care to patients with life-threatening conditions. The ASN Critical Care 2017 Early Program likely addressed many of these aspects, offering attendees insights into the latest technological advancements and clinical strategies.
[ Professional Adjustments class for senior students, Philadelphia General Hospital School of Nursing, 1949]
The rise of advanced practice nurses, including nurse practitioners and clinical nurse specialists, has further enhanced critical care nephrology. These advanced roles allow nurses to take on greater responsibilities in patient management, collaborate closely with physicians, and lead quality improvement initiatives. The expertise shared at programs like ASN Critical Care 2017 Early Program is vital for these advanced practitioners to stay at the forefront of their field.
[ Nurse with an intensive care patient, Hospital of the University of Pennsylvania, 1972]
Nursing research has become increasingly important in shaping evidence-based practice in all areas of healthcare, including critical care nephrology. Research presented and discussed at meetings like the ASN Critical Care 2017 Early Program contributes to the growing body of knowledge that informs clinical decision-making and improves patient outcomes. This emphasis on research ensures that critical care nephrology continues to advance on a solid scientific foundation.
[ 21st century nurse with patient]
As we move further into the 21st century, critical care nephrology faces ongoing challenges, including optimizing RRT delivery, managing fluid and electrolyte imbalances, and preventing complications in vulnerable patient populations. However, the field is also marked by continuous innovation and a commitment to improving patient care. Events such as the ASN Critical Care 2017 Early Program remain essential for fostering collaboration, disseminating new knowledge, and driving the future of critical care nephrology. Just as nursing has consistently adapted to meet evolving healthcare needs, critical care nephrology will continue to be a vital and dynamic field, ensuring the best possible care for critically ill patients with kidney disease.